Medical Lengthening
What is Medical Lengthening? Medical lengthening, often referred to as limb lengthening, is a surgical procedure aimed at increasing the length of bones in the limbs. This process is typically used to treat discrepancies in limb length caused by congenital conditions, injuries, or diseases. The procedure involves the use of an external fixator, such as the Ilizarov apparatus, or an internal device that gradually separates the bone segments, allowing new bone tissue to form and fill in the gap. Medical Necessity Medical lengthening is performed for several medically necessary reasons: Evaluation and Treatment Decisions The decision to proceed with medical lengthening involves a comprehensive evaluation: Acceptance within the Medical Community Limb-lengthening procedures have gained acceptance within the medical community due to advancements in surgical techniques and technology. The Ilizarov method, developed in the 1950s, revolutionized limb lengthening and has since been widely adopted. Modern techniques, such as the PRECICE nail, allow for more controlled and less invasive lengthening processes. Research and clinical outcomes support the efficacy and safety of these procedures when performed by experienced surgeons. Risks and Potential Complications As with any surgical procedure, medical lengthening carries risks and potential complications: Conclusion Medical lengthening is a critical procedure for addressing significant limb length discrepancies and improving patient function and quality of life. While it involves considerable commitment and carries risks, advancements in surgical techniques and comprehensive care have made it a viable option for many patients. Thorough evaluation and a multidisciplinary approach are essential to ensure the best outcomes.
Use of External Fixators for Damage-Control Orthopaedics in Natural Disasters
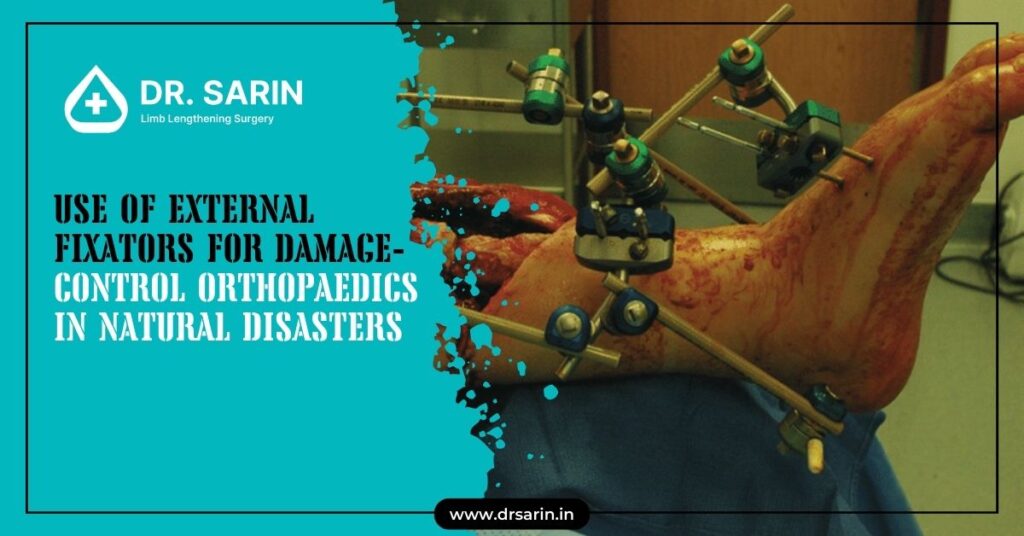
Natural disasters often lead to a surge of traumatic injuries, necessitating immediate and effective medical interventions. Among the critical tools in damage-control orthopaedics are external fixators, which play a vital role in stabilizing fractures and facilitating early mobilization in disaster environments. Purpose The primary purpose of using external fixators in natural disaster scenarios is to provide rapid stabilization of fractures. This approach helps to: External fixators are essential for maintaining the alignment of fractured bones, which is crucial in preventing complications such as infection, non-union, and disability. Methods The application of external fixators in a disaster setting follows damage-control orthopaedics principles, focusing on: In a disaster, the methods are streamlined to accommodate the often limited resources and the urgent need to treat multiple casualties. Results The use of external fixators in disaster situations has shown significant benefits, including: Patients treated with external fixators in disaster settings typically experience fewer complications and can transition to definitive care more smoothly. Materials and Methods The materials used for external fixation in disaster settings include: The methods emphasize a systematic approach: 1. Assessment: Rapid evaluation of the injury and the patient’s overall condition. 2. Preparation: Sterilization of equipment and the operative field. 3. Application: Quick yet precise placement of pins and rods to stabilize the fracture. 4. Post-application care: Monitoring for signs of infection or complications and ensuring proper alignment and stability. Technique for External Fixation Employed in the Disaster Environment The technique for applying external fixators in a disaster environment involves several key steps: 1. Initial Assessment and Triage: 2. Sterilization and Preparation: 3. Pin Insertion: 4. Frame Assembly: 5. Stabilization and Verification: 6. Post-Operative Care: Conclusion In the chaotic and resource-limited settings of natural disasters, external fixators are indispensable tools for damage-control orthopaedics. Their ability to provide rapid and effective stabilization of fractures ensures better outcomes for patients, enabling them to survive the initial trauma and recover more effectively. The techniques and methods employed are designed to be efficient and adaptable, making external fixators a critical component of disaster response and management in orthopaedic care.
Surgical Skin Preparation for Limb Lengthening Surgery

Why Is Surgical Skin Preparation Important? Surgical skin preparation removes dirt, oil, and microorganisms from the skin’s surface. This process reduces the risk of postoperative infections, which can complicate recovery and affect the overall success of the surgery. Limb lengthening procedures often involve external fixators or internal devices and require meticulous skin preparation to prevent complications. Steps in Surgical Skin Preparation Special Considerations for Surgery Conclusion Adequate surgical skin preparation is a critical component of limb lengthening surgery, directly impacting the success of the procedure and the prevention of postoperative infections. By following a systematic approach to skin preparation, including thorough cleaning, antiseptic application, and sterile draping, surgical teams can create an optimal environment for safe and successful limb-lengthening surgery. Proper patient education and adherence to postoperative care instructions enhance overall outcomes and support a smooth recovery process.
Indications for Limb Lengthening

Limb lengthening is a surgical procedure designed to correct discrepancies in limb length, restore normal function, and improve the quality of life for patients with various underlying conditions. This advanced orthopedic technique gradually stretches bone and surrounding tissues to achieve the desired length. Here are some of the primary indications for limb lengthening: Growth Plate Injuries Growth plate injuries, also known as physical injuries, can occur in children and adolescents and can lead to premature closure of the growth plate. This premature closure can result in a significant discrepancy in limb length as the unaffected limb usually grows. Limb lengthening can correct this disparity, ensuring that both limbs are of equal length and preventing associated functional impairments. Bone Infections Resulting in Leg Length Variations Severe bone infections, such as osteomyelitis, can damage bone tissue and affect the average growth of bones in children. When an infection causes part of the bone to stop growing, it can lead to leg length discrepancies. Limb lengthening surgery can help restore balance by lengthening the affected limb to match the length of the unaffected limb, thus improving overall mobility and function. Broken Bones Followed by Trauma Traumatic injuries that result in fractures can sometimes heal improperly, leading to discrepancies in limb length. This can occur when a fracture heals in a shortened position or when there is significant bone loss. Limb lengthening can correct these discrepancies by gradually stretching the shortened bone to achieve the desired length, ensuring proper alignment and function of the limb. Replacement of Missing Bone After the Surgical Removal of Bone Tumor and Fracture The surgical removal of bone tumors or treatment of severe fractures may necessitate the removal of a section of bone, resulting in a limb length discrepancy. Limb lengthening procedures can regenerate the missing bone and restore the affected limb to its average length. This process involves using specialized devices, such as the Ilizarov apparatus, to extend the bone gradually. Increasing the Stature in Dwarfs by Lengthening Both Legs For individuals with certain types of dwarfism, limb lengthening surgery can increase overall height and improve functional capabilities. This involves lengthening both legs to achieve a more proportional stature. The procedure is typically performed in stages and requires a comprehensive rehabilitation program to ensure successful outcomes and minimize complications. Conclusion Limb lengthening is a versatile and effective surgical technique to address various conditions resulting in limb length discrepancies. Whether caused by growth plate injuries, bone infections, traumatic fractures, or the need for bone replacement following tumor removal, limb lengthening can restore balance, function, and quality of life for affected individuals. Additionally, it offers a viable option for increasing stature in individuals with dwarfism. As with any surgical procedure, a thorough evaluation by an experienced orthopedic surgeon is essential to determine the appropriate indication and ensure the best possible outcome for each patient.
Available Methods Of Limb Lengthening
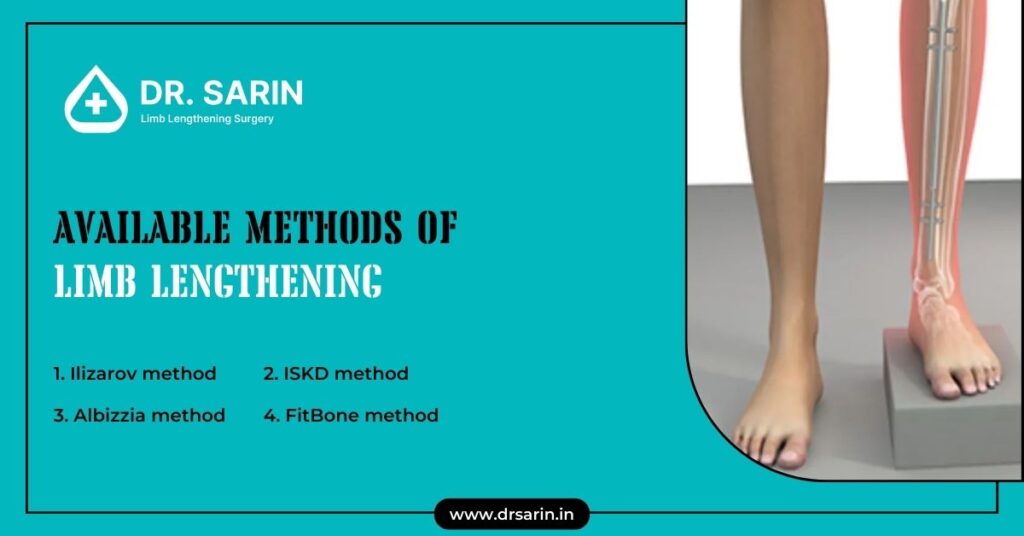
Limb lengthening is a surgical procedure designed to correct discrepancies in limb length, congenital deformities, or injuries. This advanced orthopedic technique involves cutting and gradually stretching the bone to stimulate new bone growth. Several methods are available, each with unique mechanisms and benefits. Here, we will explore the Ilizarov, ISKD, Albizzia, and FitBone methods, providing a comprehensive overview of their processes and applications. Ilizarov Method The Ilizarov method, developed by Soviet orthopedic surgeon Gavriil Ilizarov in the 1950s, is one of the most established and widely used techniques for limb lengthening. This method utilizes a circular external fixator, which consists of rings connected by adjustable rods. Procedure: Advantages: Disadvantages: ISKD Method The Intramedullary Skeletal Kinetic Distractor (ISKD) method is less invasive than external fixation devices like the Ilizarov method. Developed in the early 2000s, it involves using an internal lengthening device inserted into the bone marrow cavity. Procedure: Advantages: Disadvantages: Albizzia Method The Albizzia method, introduced by French surgeon Jean-Albert Albizzia, involves using an intramedullary nail with a ratchet mechanism. This technique also allows for internal lengthening without external fixators. Procedure: Advantages: Disadvantages: FitBone Method The FitBone method is a state-of-the-art, fully implantable limb lengthening system developed in Germany. This technique uses a motorized intramedullary nail controlled by an external remote. Procedure: Advantages: Disadvantages: Conclusion Limb lengthening methods have evolved significantly, offering patients various options tailored to their needs and conditions. The Ilizarov method remains a versatile choice for complex deformities, while the ISKD and Albizzia methods provide less invasive alternatives with internal devices. The FitBone method represents the latest advancement, combining precision with patient comfort. Each technique has its advantages and challenges, and the choice of method depends on factors such as the patient’s condition, the surgeon’s expertise, and the desired outcome.
Poliomyelitis Treatment with leg lengthening ilizarov method
Poliomyelitis, commonly known as polio, can lead to muscle weakness and paralysis. It often affects the legs and results in limb length discrepancies. The Ilizarov method, a specialized orthopedic technique, offers a poliomyelitis treatment option for correcting leg deformities and length inequalities caused by polio. This article provides an overview of the treatment for polio affected leg, including patient selection, operative techniques, post-operative management, and outcomes. Patients and Methods The Ilizarov method for treating poliomyelitis-induced leg deformities is typically considered for patients who have completed their growth and exhibit significant limb length discrepancies or deformities. Patient evaluation includes a thorough assessment of medical history, physical examination, imaging studies, and functional status to determine the suitability for surgery. Operative Technique: Closed Method The closed method involves using external fixation devices, such as the Ilizarov apparatus, to gradually lengthen and treat the polio-affected leg. The procedure may also include stabilizing the foot by arthrodesis, which involves fusing the joints to improve stability and function. Operative Technique: Open Treatment with Osteotomies Open surgical procedures may sometimes be necessary to correct complex deformities or achieve desired limb alignment. Post-operative Management Following surgery, patients undergo a comprehensive rehabilitation program aimed at maximizing function, reducing pain, and preventing complications. This may include physical therapy, occupational therapy, and assistive devices to support mobility and independence during recovery. Results The outcomes of Ilizarov treatment for treatment for polio affected leg vary depending on the severity of the deformities, patient factors, and adherence to post-operative protocols. Overall, the Ilizarov method offers a promising approach for correcting limb length inequalities and deformities caused by polio, improving affected individuals’ function and quality of life. The Ilizarov method provides a valuable poliomyelitis treatment for addressing leg length discrepancies and deformities resulting from poliomyelitis. Through meticulous patient selection, precise operative techniques, and comprehensive post-operative care, orthopedic surgeons can help patients with polio achieve improved limb alignment, function, and overall well-being.
Can Height Be Increased after 21?

The question, can height be increased after 21 is common, especially for individuals who may be dissatisfied with their current stature. While height increase is typically most significant during the growth spurt of puberty, there are still possibilities for height enhancement beyond this stage. This article explores the potential, can height grow after 21 and examines various factors that may influence growth in adulthood. Height Increase after Puberty Although most height growth occurs during puberty when growth plates in the long bones are still open, some individuals may experience additional height gain into early adulthood. However, the potential for a significant height increase diminishes with age as the growth plates fuse and bone development decreases. Eating Healthy: Can height grow after 21? While nutrition plays a crucial role in overall health and development, there is limited evidence suggesting that specific foods or dietary practices can increase height in adults. However, maintaining a balanced diet rich in essential nutrients such as protein, calcium, vitamin D, and other micronutrients can optimize bone health and support overall growth and development. Are Medicines to increase height after 21 and Hormonal Injections Effective? Height growth medicine and hormonal injections are sometimes prescribed for individuals with growth hormone deficiencies or certain medical conditions affecting growth. Medicine to increase height after 21 may stimulate growth by increasing the production of growth hormones or addressing underlying hormonal imbalances. However, their effectiveness varies depending on individual factors and medical indications, and they may only be suitable or practical for some. How To Increase Height After 21? Height increase after 21 (puberty) is primarily influenced by posture, spinal alignment, and bone density. Improving posture through exercises that strengthen core muscles and promote spinal alignment can create the illusion of height and maximize overall stature. Maintaining a healthy lifestyle, including regular exercise, adequate sleep, and proper nutrition, can also support bone health and optimize growth potential. While the potential, can height be increased after 21 diminishes after puberty, modest height enhancement is still possible in early adulthood. Healthy lifestyle habits, including maintaining a balanced diet, practicing good posture, and engaging in regular exercise, can support overall growth and well-being. However, it’s essential to approach height enhancement with realistic expectations and consult a healthcare professional like Dr. Sarin for personalized advice and guidance.
Average Height For A Man In India 2024

In 2024, the average height for a man of individuals in India reflects a diverse range influenced by various factors. Understanding the factors affecting the average height in India provides valuable insights into the dynamics of physical growth and development within the Indian population. Height of Normal Man: Indian Chart Average Height for a Man in India varies across regions, ethnicities, socioeconomic backgrounds, and other demographic factors. While there is no singular “Indian average height,” studies have reported average heights ranging from approximately 5 feet 3 inches to 5 feet 6 inches for adult males and 4 feet 9 inches to 5 feet 2 inches for adult females. These averages may vary based on the population studied and the methodology used to collect height data. Factors Affecting Average Height in India Several factors contribute to the variation in average height in India observed among individuals: 1. Genetics: Genetic factors play a significant role in determining an individual’s height. Variations in genetic traits inherited from parents can influence height potential, with specific populations exhibiting taller or shorter average heights due to genetic predispositions. 2. Nutrition: Adequate nutrition is crucial for optimal growth and development during childhood and adolescence. Malnutrition, micronutrient deficiencies, and poor dietary practices can stunt growth and lead to shorter stature in adulthood. Access to nutritious food, especially during critical periods of growth, significantly impacts average height within populations. 3. Healthcare: Access to healthcare services, including prenatal care, pediatric care, and disease prevention programs, can influence growth trajectories and overall health outcomes. Improved healthcare infrastructure and healthcare-seeking behavior contribute to better health and nutrition outcomes, potentially leading to taller average heights for a man in specific regions or populations. 4. Socioeconomic Factors: Socioeconomic status, including income, education, and living conditions, can affect access to resources essential for healthy growth and development. Individuals from higher socioeconomic backgrounds may have better access to nutritious food, healthcare services, and environmental conditions conducive to growth, contributing to taller average heights within those populations. 5. Environmental Factors: Environmental factors such as pollution, climate, and urbanization can impact health and well-being, potentially influencing growth patterns and average female height. Urban areas may experience different growth trends compared to rural areas, reflecting variations in lifestyle, diet, and exposure to environmental stressors. 6. Ethnic Diversity: India is characterized by significant ethnic and cultural diversity, with distinct populations exhibiting unique genetic traits and growth patterns. Ethnic differences in average height may reflect genetic variations, historical influences, and cultural practices specific to each group. The average height for a man of individuals in India in 2024 reflects a complex interplay of genetic, environmental, socioeconomic, and healthcare factors. While there is no single “average height in India”, understanding the diverse factors shaping physical growth and development provides valuable insights into population health and well-being. Efforts to address nutrition, healthcare access, socioeconomic disparities, and environmental challenges are essential for promoting optimal growth and achieving healthier height outcomes across the Indian population.
Are There Any Height Increase Pills to foster height Growth?
Height is primarily determined by genetics and influenced by various factors such as nutrition, environment, and hormonal balance. While no drugs are specifically designed to increase height growth in adults, specific treatments may be prescribed for individuals with growth hormone deficiencies or other medical conditions affecting growth. In this comprehensive guide, we’ll explore the potential for height growth medicine during childhood and adolescence and options for increasing height after puberty. Increasing Height During Childhood and Adolescence During childhood and adolescence, the body undergoes significant growth and development, primarily driven by the release of growth hormones produced by the pituitary gland. Adequate nutrition, proper sleep, and regular physical activity support optimal growth during this period. Children with growth hormone deficiencies may be prescribed synthetic injections or height growth medicine to stimulate growth and achieve typical height milestones. Increasing Height after Puberty After puberty, when growth plates in the long bones of the body fuse and stop growing, it becomes challenging to increase height through natural means. However, limited options for increasing height in adults with certain medical conditions may exist. For example, individuals with growth hormone deficiencies or skeletal dysplasias may benefit from height growth supplements or growth hormone therapy or orthopaedic surgeries to correct bone deformities and improve stature. Height Increasing Supplements: Use with Caution While height increasing supplements and medicines may sound appealing, their effectiveness is limited to specific situations. For children with conditions affecting human growth hormone (HGH) production, doctors might recommend synthetic HGH supplements. Similarly, older adults at risk of osteoporosis may benefit from vitamin D or calcium supplements. However, for the general population, these supplements offer false promises. Once growth plates fuse, usually after puberty, height increase becomes impossible regardless of supplement claims. Therefore, it is crucial to approach height increasing supplements and height increase medicines with caution and skepticism, and always consult a healthcare professional before use. Are Height Increase Pills Safe? Height growth pills, supplements, or herbal remedies marketed as “height enhancers” or “growth stimulators” are widely available in the market but lack scientific evidence to support their effectiveness or safety. These height growth capsule often contain a combination of vitamins, minerals, amino acids, and herbal extracts purported to promote growth. However, height growth supplements efficacy and safety remain questionable, and they may pose risks such as adverse reactions, interactions with medications, or unknown long-term effects. It’s essential to consult with a healthcare professional before using any height growth medicine or supplements, especially in children and adolescents. How Can Height Be Increased After Puberty? While it’s challenging to increase height after puberty, there are lifestyle modifications and interventions that may help optimize posture and maximize height potential. These include: 1. Maintaining good posture: Proper posture can create the illusion of height and prevent spinal compression, contributing to height loss over time. Practising exercises that strengthen the core muscles and improve spinal alignment can help maintain optimal posture. 2. Healthy lifestyle habits: Healthy lifestyles such as eating a balanced diet rich in calcium and vitamin D, regular exercise, and ensuring adequate sleep can support overall health and well-being. While these practices may not directly increase height, they can optimize bone health and promote overall growth and development. 3. Consulting a healthcare professional: Individuals concerned about their height or seeking interventions to maximize height potential should consult a qualified healthcare professional, such as an endocrinologist or orthopaedic specialist. These specialists can assess individual growth patterns, identify underlying factors contributing to short stature, and recommend appropriate interventions or treatments. The only possible way to increase height after puberty is through limb lengthening surgery. However, this surgery is a severe surgical operation, and it is essential to obtain detailed information about the process from a specialist doctor before making this decision. One of the points we are most sensitive about is ensuring that our patients are correctly informed about the process. Individuals considering surgery are first subjected to health examinations by our specialist doctor. These examinations include checking the general health status, blood tests, X-ray images, bone health, and muscle structure. Additionally, the patient’s age and any chronic conditions are considered; based on these, our doctor decides whether the patient is suitable for surgery. Contact our patient representatives directly if you want detailed information about limb lengthening surgery.
Lengthening In Four Segments

Lengthening procedures are intricate orthopedic surgeries designed to address limb length discrepancies and deformities, enhancing function and improving the quality of life for patients. This comprehensive guide explores the various segments involved in lengthening procedures, from deformity correction to the consolidation phase. Deformity Correction Deformity correction is the initial stage of lengthening procedures, focusing on addressing any structural abnormalities or malformations in the affected limb. This may involve realigning bones, correcting angular deformities, or addressing congenital anomalies. Advanced imaging techniques, such as X-rays and MRI scans, are used to assess the extent of the deformity and guide surgical planning. During this segment, the orthopedic surgeon carefully evaluates the patient’s unique anatomy and develops a customized treatment plan to achieve optimal correction. Humeral Lengthening Humeral lengthening specifically targets the upper arm bone (humerus), addressing conditions such as congenital shortening, trauma-related defects, or acquired deformities. The lengthening process involves carefully controlled distraction of the bone using specialized external fixation devices or internal lengthening nails. By gradually elongating the humerus over a prescribed period, surgeons can achieve significant gains in limb length and restore symmetry to the upper extremity. Close monitoring and regular follow-up appointments are essential during the lengthening process to ensure proper bone healing and minimize complications. Distraction Phase The distraction phase is a critical component of lengthening procedures, during which controlled mechanical forces are applied to the bone to stimulate new bone formation and elongation. This phase typically begins several days after the initial surgical procedure and continues over several weeks or months, depending on the desired amount of lengthening. External fixation devices or internal lengthening nails are adjusted periodically to gradually separate the bone segments and promote the formation of new bone tissue. Patients may experience discomfort or pain during the distraction phase, which can be managed with appropriate pain management techniques and close supervision by the healthcare team. Consolidation Phase Once the desired lengthening is achieved, the consolidation phase begins, focusing on stabilizing the newly formed bone and promoting bone healing. During this phase, the distraction devices or lengthening nails are locked in place to prevent further movement of the bone segments. The patient is closely monitored for signs of bone healing, such as callus formation and radiographic evidence of bone union. Physical therapy and rehabilitation exercises may be initiated to restore strength and function to the affected limb. The consolidation phase is crucial for ensuring the long-term success of the lengthening procedure and minimizing the risk of complications, such as delayed union or non-union of the bone. Conclusion Lengthening procedures are complex orthopedic surgeries that involve multiple segments, from deformity correction to the consolidation phase. By addressing structural abnormalities and carefully controlling bone elongation, Limb Lengthening surgeons can achieve significant improvements in limb length and function for patients with congenital or acquired limb length discrepancies. Close collaboration between patients, orthopedic surgeons, and healthcare providers is essential throughout the lengthening process to optimize outcomes and ensure a successful recovery.

