Limb Lengthening Surgery in India | Why International Patients Choose Dr. Sarin

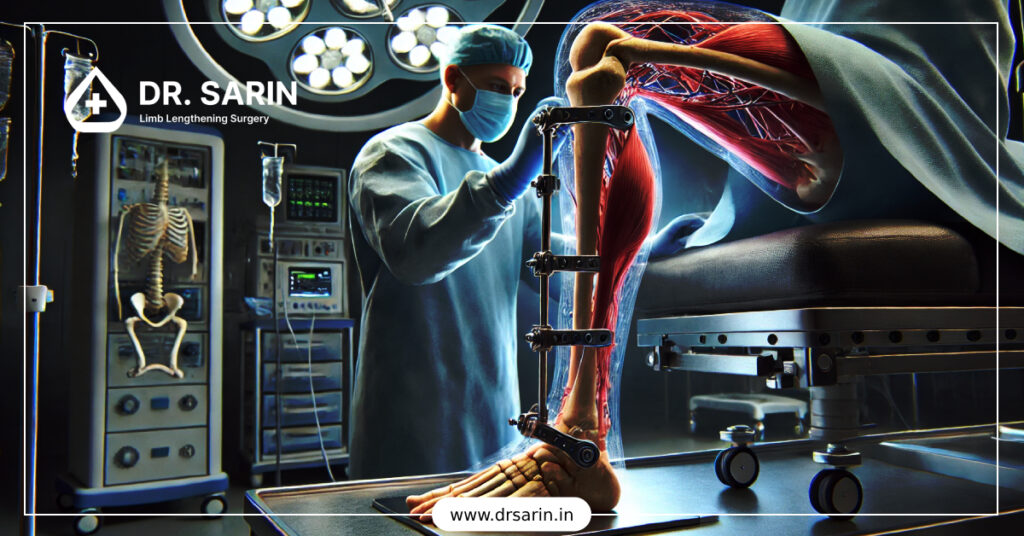
Limb Lengthening Surgery in India: Why International Patients Choose Dr. Sarin: In recent years, India has become a global hub for advanced medical treatments, including limb lengthening surgery, a life-changing procedure for patients with height concerns, limb deformities, or leg length discrepancies. Among the leading names in this field, Dr. Amar Sarin stands out as a trusted expert for both Indian and international patients. So, why do people from across the world travel to India, and specifically to Dr. Sarin’s clinic, for limb lengthening? Here’s everything you need to know. A Growing Global Demand for Limb Lengthening Limb lengthening surgery has moved beyond correcting deformities. Today, many patients also seek the procedure for: Correcting congenital or post-traumatic limb length discrepancies Improving posture, balance, and gait Enhancing self-confidence through cosmetic height increase However, in countries like the USA, UK, or Germany, the procedure is often expensive, hard to access, and has longer waiting times. India offers affordability, shorter waitlists, and globally recognized surgical expertise, a perfect combination for international patients. Why Choose Dr. Amar Sarin? 1. Over 3,000 Limb Lengthening Surgeries Performed With 30+ years of surgical experience, Dr. Sarin is one of India’s most seasoned orthopedic surgeons specializing in limb lengthening and deformity correction. He has successfully treated patients from over 25 countries. 2. Advanced Techniques with Global Standards Here are some available methods for limb lengthening: Ilizarov External Fixator PRECICE 2.2 Magnetic Nail (Remote Controlled) FitBone & ISKD Internal Nails Deformity Correction with Taylor Spatial Frame (TSF) These are the same devices used in top-tier hospitals in Europe or the U.S., but at a fraction of the cost. 3. Comprehensive Pre- and Post-Operative Care From visa assistance and airport pick-ups to pre-surgical tests and daily physiotherapy, Dr. Sarin’s clinic provides end-to-end support for international patients. Every international patient receives: Personalized treatment planning Private hospital accommodation options English-speaking support staff Telemedicine follow-ups after discharge Cost Advantage Without Compromising Quality Limb lengthening surgery abroad can cost between $75,000 to $150,000. In India, Dr. Sarin offers the same procedures for 1/4th of the price, with: International-standard equipment Board-certified surgical team Fully equipped, NABH-accredited hospital facilities Patients often combine the surgery with short-term stays in India, making it a cost-effective and medically sound option. Smooth Travel & Recovery for International Visitors Dr. Sarin’s team offers assistance with: Medical visa invitations Airport transfers and hotel coordination Customized post-op rehabilitation plans Travel insurance guidance (if applicable) Patients from the UAE, U.S., UK, Canada, Nigeria, Australia, and Europe have successfully undergone treatment with minimal travel stress. Real Patient Experiences “Transformative experience! Dr. Sarin’s limb lengthening gave me a new perspective. Expertise and care beyond compare.” — Ahmed, Iraq “I came from London to get my height increased by 6 cm. Dr. Sarin and his team were incredibly professional and kind throughout my 9-month journey.” — James R., UK Final Thoughts If you’re considering Hight lengthening surgery and seeking world-class outcomes at a reasonable cost, Dr. Amar Sarin in India offers the ideal solution. His experience, technology, and patient-first philosophy make him a trusted name for international patients. Ready to Take the First Step? Contact Dr. Sarin’s clinic today to schedule a video consultation or learn more about the treatment packages available for international patients. Contact Us at +919810376803 or Book free consultation now!
What Conditions Can Limb Lengthening Surgery Effectively Treat?

Limb lengthening surgery is a specialized orthopedic procedure used to increase the length of bones, typically in the legs or arms, and can effectively treat several medical and cosmetic conditions. Below is a concise overview of conditions it addresses, based on medical insights and standard practices: Conditions Treated by Limb Lengthening Surgery 1. Congenital Limb Length Discrepancy: Description: Conditions present at birth, such as congenital short femur, fibular hemimelia, or proximal femoral focal deficiency, where one limb is shorter than the other. Effectiveness: Surgery equalizes limb lengths, improving function, gait, and reducing compensatory issues like scoliosis or joint pain. 2. Acquired Limb Length Discrepancy: Description: Discrepancies caused by trauma (e.g., fractures), infections (e.g., osteomyelitis), or growth plate injuries that impair bone growth. Effectiveness: Restores symmetry, enhances mobility, and prevents long-term complications like arthritis or back pain. 3. Short Stature Disorders: Description: Genetic or endocrine conditions like achondroplasia (a common form of dwarfism), Turner syndrome, or hypochondroplasia, where individuals have disproportionately short limbs or overall height. Effectiveness: Increases height (often 6–12 inches in achondroplasia) and improves limb proportions, enhancing physical function and quality of life. 4. Bone Deformities: Description: Conditions like bowlegs (genu varum), knock-knees (genu valgum), or rotational deformities often associated with skeletal dysplasias or trauma. Effectiveness: Corrects angular deformities while lengthening bones, improving alignment and weight-bearing capacity. 5. Nonunion or Malunion Fractures: Description: Bones that fail to heal properly (nonunion) or heal in a misaligned position (malunion) after fractures. Effectiveness: Stimulates bone regeneration and corrects length or alignment, restoring function. 6. Bone Defects or Loss: Description: Loss of bone due to tumors, infections, or severe trauma, creating gaps or shortened segments. Effectiveness: Regenerates bone through distraction osteogenesis, filling gaps and restoring limb length. 7. Cosmetic Height Enhancement: Description: Elective lengthening for individuals seeking increased height due to personal or social reasons, without underlying medical conditions. Effectiveness: Can add 2–6 inches in height, improving self-esteem, though it carries risks and requires careful psychological evaluation. Procedure, Effectiveness Factor, Risks Procedure: Limb lengthening or height increase surgery typically involves cutting the bone (osteotomy), attaching an external fixator or internal device (e.g., PRECICE nail), and gradually lengthening the bone through distraction osteogenesis (1 mm/day). The process includes lengthening and consolidation phases, lasting months. Effectiveness Factors: Success depends on patient age, bone quality, compliance with physical therapy, and surgeon expertise. Children and adolescents often achieve better outcomes due to active growth plates. Risks: Includes infection, nerve damage, joint stiffness, or prolonged recovery, requiring careful patient selection and postoperative care. Specific Considerations Achondroplasia: Lengthening is common for arms and legs to improve reach and mobility, often performed in stages. Limb Discrepancy: Effective for discrepancies >2 cm, where shoe lifts are insufficient. Cosmetic Cases: Controversial due to high costs (₹10–50 lakh in India) and risks; not covered by insurance. If you’re considering this surgery for a specific condition or have a case in mind (e.g., for yourself or someone else), please share more details, and I can provide insights or guide you on next steps, such as finding specialists in India.
Average Height of UK 2025

The average height of a population serves as a key indicator of overall health and nutrition levels within a country. In the UK, this metric has shown a steady increase over the years, driven by improvements in living conditions, advancements in healthcare, and enhanced dietary habits. Understanding these trends not only provides insight into public health but also informs policies aimed at fostering a healthier future. Current Average Height of UK (2025) As of 2025, the average height for adults in the UK is as follows: These figures represent a gradual rise over recent decades, reflecting the positive impact of various societal factors. Factors Affecting Average Height in the UK Several elements contribute to the average height of individuals in the UK: Historical Trends in Height Over the past century, historical data indicates a consistent increase in average height across the UK. This trend can be attributed to enhanced living standards, medical advancements, and improved nutrition. Notably, the post-World War II era saw significant improvements in public health policies, which have had lasting effects on population height. Regional Variations While national averages provide a broad overview, there are regional variations in average height within the UK. These differences can be influenced by local dietary habits, socioeconomic conditions, and genetic diversity. For example, studies have shown that individuals in urban areas may have different average heights compared to those in rural regions, often due to lifestyle and dietary differences. The Impact of Global Trends In addition to local factors, global trends such as increased migration and cultural exchange can influence dietary habits and health practices, potentially affecting average height. As the UK becomes more multicultural, the blending of dietary practices may lead to new health outcomes. Conclusion Understanding the average height and the factors that influence it is essential for developing policies aimed at improving public health and nutrition. By addressing these areas, we can continue to support the positive trend in average height and overall well-being in the UK. As we move forward, ongoing research and community engagement will be crucial in ensuring that all individuals have the opportunity to reach their full height potential, contributing to a healthier society overall. Additional Resources For those interested in exploring this topic further, consider the following resources: NHS Guidelines on Nutrition: NHS Nutrition Public Health England Reports on Height Trends: PHE Reports Research on Genetics and Height: Genetics Home Reference
Can I Still Run After Height Increase Surgery?

Yes, you can still run after height increase (limb lengthening) surgery, but only after a full recovery, which usually takes 6 to 12 months. With proper physiotherapy and rehabilitation, most patients regain normal mobility and can return to activities like jogging or running, though high-impact sports may require extra caution. For many individuals considering limb lengthening surgery, one of the most common concerns is whether they can continue leading an active lifestyle post-surgery. Running, walking, gym workouts, and even playing sports are essential parts of many lives, and this article breaks down what to expect after height increase surgery and how to safely return to running. Understanding Limb Lengthening Surgery Limb lengthening surgery is a complex orthopedic procedure that gradually increases bone length using advanced internal or external devices. Most commonly performed on the femur or tibia, the surgery involves cutting the bone and slowly separating it to allow new bone to form in the gap, a process known as distraction osteogenesis. While the surgery is effective in increasing height, it temporarily impacts mobility, muscle function, and overall biomechanics, which directly influences the ability to walk, jog, or run during the recovery period. The Recovery Timeline for Running Recovery from limb lengthening surgery typically occurs in several stages: Initial Healing Phase (0–3 months): Focus is on pain management, wound care, and limited mobility. Bone Consolidation Phase (3–6 months): Bone becomes stronger, and patients begin using assistive devices like walkers or crutches. Rehabilitation & Physiotherapy (6–12 months): Intensive physiotherapy helps rebuild strength, balance, coordination, and endurance. Return to Running (>12 months): With medical clearance, many patients can gradually return to low-impact jogging and later resume full running. The Role of Physiotherapy in Returning to Running A structured physiotherapy plan is crucial for regaining muscle flexibility, joint mobility, and gait balance. Therapists often incorporate: Stretching and strengthening exercises Gait training Balance and coordination drills Gradual weight-bearing activities These efforts ensure a smoother and safer return to running. Caution with High-Impact Sports While recreational running is usually possible post-surgery, contact sports or intense running (like marathons or sprints) may need extra care. Surgeons often recommend waiting until bone density and muscular strength are fully restored, sometimes 18 months post-op. Listening to your body, avoiding overexertion, and following professional guidance are key to avoiding injury. Tips for a Safe Comeback to Running Always get clearance from your orthopedic surgeon. Start with low-impact activities like swimming or cycling. Use proper running shoes with cushioning. Avoid uneven terrain in early stages. Follow up regularly for X-rays and assessments. Final Thoughts Height increase surgery doesn’t have to mean giving up your active lifestyle. With patience, commitment to physiotherapy, and ongoing support from your medical team, you can safely get back to running and even thrive in your post-surgery body. The journey may be long, but the results, both in height and mobility, can be life-changing.
Why Height Increases Stop After 18?: A Biological Overview

Most people stop growing taller after the age of 18. But why does height increase stop at this point? Is there a biological cut-off, or can you still grow after 18 naturally? In this article, we’ll take a closer look at the scientific and biological processes behind height growth, why it stops, and whether there are any exceptions to this rule. The Science of Height: How Do We Grow Taller? Height growth is primarily influenced by the long bones in your arms and legs. These bones grow due to a special area of cartilage near their ends called the epiphyseal growth plates (or simply, growth plates). Key factors in height growth: Growth Plates: Found near the ends of long bones, responsible for bone lengthening. Human Growth Hormone (HGH): Stimulates growth plates. Sex Hormones (Estrogen & Testosterone): Help regulate the closure of growth plates during puberty. What Happens After 18? By the time you reach late adolescence (usually between 16 to 21 years), your growth plates begin to close or fuse. Once they’re closed, no more bone lengthening can occur, meaning your height becomes permanently fixed. Here’s what causes growth to stop: Growth Plate Fusion: Cartilage is replaced by solid bone, halting further elongation. Decline in HGH: Natural production of growth hormone decreases with age. Increased Estrogen/Testosterone: These hormones accelerate plate closure during puberty. Fun Fact: In both boys and girls, estrogen is the primary hormone that leads to growth plate closure—even in males! Can You Grow After 18? In very rare cases, some individuals may experience minimal height growth up to 21–22 years, particularly males who had late-onset puberty. However, this growth is usually limited to 1–2 cm and not common. Common myths: ❌ Stretching will not increase height after 18. ❌ Supplements cannot reopen growth plates. ✅ Limb Lengthening Surgery is the only proven way to increase height after plate closure. How to Know If Your Growth Plates Are Still Open? The only accurate way is through a bone X-ray (typically of the wrist or knee). Doctors check for open growth plates using a method called the Greulich and Pyle atlas, which compares bone age to chronological age. Can Exercise, Nutrition or Posture Help? While these won’t increase your bone length after 18, they can help you: Improve posture → appear taller Strengthen your core → enhance spinal alignment Maintain good bone health → prevent height loss with age Tips for maximizing height potential (before 18): Eat a protein-rich, calcium-packed diet Sleep 8–9 hours regularly Avoid steroids or early puberty triggers Engage in height-promoting activities (swimming, basketball, sprinting) What If You Still Want to Increase Your Height After 18? If you’re over 18 and serious about gaining height, your only medically-approved and scientifically-backed option is limb lengthening surgery. This procedure can add 5–8 cm or more to your height using either internal or external fixation devices. Explore more: Limb Lengthening Surgery: How Much Height Can You Safely Gain? Conclusion To sum it up, your height stops increasing after 18 because your growth plates close, a process driven by puberty hormones. While small exceptions exist, natural height growth past 18 is extremely rare. For those still seeking to grow taller, modern surgical methods may offer a solution. FAQs Q. Can I still grow taller at 19 or 20?A. Rarely, and only if your growth plates haven’t fused. A bone X-ray can confirm this. Q. Is there any medicine to reopen growth plates?A. No proven medicine or supplement can reopen fused growth plates. Q. Can limb lengthening increase height after 21?A. Yes. This is currently the only effective method post-growth plate closure.
Height Increase Surgery Complications

Height Increase Surgery Complications: Understanding the Risks Involved in Limb Lengthening Procedures Height increase surgery—also known as limb lengthening surgery—has grown in popularity among individuals seeking not only to correct limb discrepancies but also to improve self-confidence and quality of life. While it offers life-changing benefits, it’s essential to understand that the procedure is complex and comes with potential complications. As with any major surgical intervention, being informed about the risks is just as important as knowing the benefits. This guide offers an overview of the common and rare complications associated with height increase surgery and highlights the importance of expert care in minimizing them. What Is Height Increase Surgery? Height increase surgery is based on the technique of distraction osteogenesis, where the bone is surgically cut and gradually lengthened using an external or internal device. Over time, new bone, muscle, and tissue grow in the gap, allowing for an increase in height. While advancements in technology have made the procedure safer and more predictable, it still involves significant strain on the body, particularly the musculoskeletal and nervous systems. Common Complications After Height Increase Surgery 1. Pain and Discomfort Pain is a natural response post-surgery, especially during the distraction phase. If not managed well, it can affect mobility, sleep, and mental health. Proper pain management plans are essential to keep discomfort at bay. 2. Joint Stiffness Muscles, tendons, and ligaments are also being stretched. Without proper physiotherapy, stiffness in the ankle, knee, or hip joints may occur. Regular stretching and guided physical therapy help minimize this risk. 3. Nerve Irritation or Damage Nerves may be stretched along with the bones. This can lead to numbness, tingling, or weakness. In rare cases, nerve damage can be long-term, but this is typically avoidable with proper monitoring. 4. Delayed Bone Healing Sometimes the new bone doesn’t regenerate as quickly as expected. Poor nutrition, smoking, or inadequate rest can contribute to this issue. Additional procedures or bone grafting may be required in such cases. 5. Muscle Tightness and Cramps Muscles may not adapt as quickly as bone. This can result in tightness, spasms, or even temporary deformities. Ongoing physical therapy and muscle relaxants help alleviate this. Less Common But Serious Complications 1. Infection External fixators increase the risk of pin-site infections. Internal rods lower this risk but still carry a chance of deep tissue infections. Daily hygiene and regular check-ups help prevent infections. 2. Bone Deformity or Misalignment If the bone grows at an uneven angle, deformity can occur. Skilled surgical planning and real-time monitoring during the process are critical to avoid this. 3. Psychological Stress The long recovery time and physical limitations can lead to depression or anxiety. Emotional support and counseling are an important part of the journey. How to Minimize Risks? Choosing the right surgeon and medical team plays a vital role in reducing complications. Here’s what to look for: Board-certified orthopedic surgeon with experience in limb lengthening Transparent discussion of risks and outcomes A strong post-op support system: physiotherapists, pain management, nutritionists Regular follow-ups for monitoring bone growth and alignment Importance of Post-Surgery Rehabilitation Rehabilitation is not optional—it is part of the healing process. Physiotherapy: Keeps joints mobile and muscles flexible Nutrition: Supports bone healing and tissue growth Lifestyle Adjustments: Adequate rest, avoiding smoking and alcohol, and stress management Mental Health Care: Coping with limitations during recovery can be challenging—support groups and therapy help Is It Worth the Risk? Height increase surgery can be transformative for individuals with medical or psychological reasons for pursuing it. But it’s crucial to have realistic expectations and be fully committed to the lengthy recovery process. With expert guidance, complications are rare and manageable. However, patients should always weigh the risks and rewards and consult a qualified specialist before making a decision. Final Thoughts Height increase surgery is not just about gaining inches—it’s a complex medical journey. Understanding the complications and preparing for them is essential to ensure the best outcomes. Dr. Amar Sarin, one of India’s most trusted limb lengthening specialists, prioritizes patient education, transparent guidance, and holistic post-surgical care. If you’re considering this path, take the time to learn, plan, and choose your medical partner wisely.
Pain Management After Limb Lengthening Surgery | Dr. Sarin India

Limb lengthening surgery is a life-changing procedure that can dramatically improve physical appearance, posture, self-esteem, and even mobility in some cases. However, like any major orthopedic intervention, it comes with its own set of challenges—pain management being one of the most crucial aspects of recovery. As a limb lengthening specialist in India, I, Dr. Amar Sarin, understand how important it is to educate patients not just about the surgery, but about what happens afterward. Managing pain effectively not only improves the overall experience but also promotes faster recovery and better outcomes. Why Does Pain Occur After Limb Lengthening Surgery? Limb lengthening involves a controlled and gradual process of bone separation and new bone formation, also known as distraction osteogenesis. During this time: Bones are slowly pulled apart Muscles, nerves, tendons, and soft tissues stretch along with the bone The body works to heal and generate new tissue These processes can naturally cause discomfort, tightness, and pain, especially during the distraction and early consolidation phases. However, with the right strategies, pain can be kept within manageable limits. My Approach to Pain Management Every patient experiences pain differently, so I focus on creating a personalized pain management plan for each individual. Here’s how we manage post-operative pain step-by-step: 1. Pre-Surgery Counseling and Planning Pain management begins before the surgery. I ensure that all my patients are: Mentally prepared for what to expect Educated on pain scales and how to communicate discomfort Introduced to our pain management team who will support them throughout recovery 2. Medications for Pain Relief We use a multi-modal approach to minimize reliance on any one medication. This includes: NSAIDs (Non-Steroidal Anti-Inflammatory Drugs): Help reduce inflammation and mild to moderate pain. Opioids (used cautiously): Reserved for short-term, severe pain during the early recovery phase. Neuropathic Pain Agents: For nerve-related discomfort that may arise during limb stretching. Muscle Relaxants: To reduce spasms and tension during physiotherapy. We adjust medication doses based on the patient’s age, pain threshold, and progress. 3. Physical Therapy and Stretching Pain often increases when movement decreases. That’s why physiotherapy is vital. It: Improves flexibility and range of motion Reduces stiffness and muscle tension Prevents contractures and joint issues I work closely with trained physiotherapists who guide gentle exercises tailored to each recovery stage. Movement may feel uncomfortable at first, but over time, it actually reduces pain and accelerates healing. 4. Distraction Schedule and Rate Control One of the most important aspects of pain management is controlling the distraction rate—the speed at which the bones are being lengthened. If the bone is lengthened too quickly, pain increases and complications may arise. I monitor X-rays and pain feedback closely to adjust the distraction rate safely, ensuring progress without triggering unnecessary discomfort. 5. Non-Medical Pain Relief Techniques Complementary therapies often help patients cope better. These include: Cold packs to reduce swelling and numb the area Heat therapy to relax tight muscles Guided meditation and breathing techniques Distraction methods such as music, reading, or light entertainment Support groups or one-on-one sessions with previous patients to boost emotional strength Pain is not just physical—it’s also emotional. We treat the whole person, not just the symptoms. 6. Emotional and Psychological Support Living through limb lengthening is a journey of endurance. Anxiety, frustration, and emotional fatigue can amplify physical pain. That’s why I always encourage: Open communication between patient, family, and the medical team Regular check-ins with a mental health counselor Creating a realistic recovery timeline to set proper expectations When patients feel emotionally supported, their ability to manage pain increases significantly. 7. Transition to Home-Based Recovery Once patients are discharged, they’re provided with: A detailed medication and physiotherapy plan 24/7 support via call or consultation for any flare-ups Regular virtual check-ups or in-clinic visits Guidance on daily activity, diet, and sleep to naturally support healing Final Thoughts from Dr. Amar Sarin Pain after limb lengthening surgery is real, but it is also manageable. With a well-structured plan, emotional support, and consistent follow-up, most patients find that their pain becomes less intense over time—and completely worth the transformation they achieve. If you or your loved one is considering limb lengthening surgery, know that you will never walk the road alone. My team and I are here to guide you through every step of the journey, helping you rise stronger, taller, and pain-free. Need Help or Have Questions? Schedule a consultation, and let’s discuss how we can make your transformation smooth and supported—with expert care and a personalized pain management plan.
Exercise & Recovery After Limb Lengthening Surgery: What You Must Know?

Recovery after limb lengthening surgery is just as important as the procedure itself. Physical therapy and controlled exercise play a crucial role in helping patients regain strength, flexibility, and mobility. However, improper exercise or premature physical activity can lead to complications. In this blog, we will explore the do’s and don’ts of exercising after limb lengthening surgery to ensure a smooth and successful recovery. The Initial Recovery Phase: What to Expect After limb lengthening surgery, patients undergo a gradual bone distraction process, which typically lasts 3 to 6 months. During this period, mobility is limited, and proper care is necessary to avoid complications. Here’s what to expect in the early recovery phase: Mild to moderate pain – This is managed with medications and therapy. Swelling and stiffness – Common in the first few weeks but gradually reduces with movement. Gradual mobility training – Guided movement to prevent joint stiffness. Do’s of Exercise After Limb Lengthening Surgery Engaging in the right type of exercise can accelerate recovery and improve flexibility. Here are some essential do’s: Start with light stretching – Helps maintain muscle flexibility. Follow doctor-prescribed physiotherapy – Tailored exercises assist in muscle recovery. Low-impact activities – Swimming and cycling can improve circulation and mobility. Use resistance bands – Strengthens muscles without putting stress on healing bones. Don’ts of Exercise After Limb Lengthening Surgery Some activities can be harmful during recovery and should be avoided: Avoid high-impact exercises – Running, jumping, and heavy weightlifting can strain healing bones. No overexertion – Excessive movement can delay bone regeneration. Skipping physiotherapy – Neglecting guided therapy can result in stiffness and loss of mobility. Ignoring pain signals – Pain is an indicator of potential strain; always listen to your body. How Physiotherapy Helps in Recovery Physiotherapy is an essential part of post-surgery rehabilitation. It helps by: Improving blood circulation – Enhances healing. Restoring range of motion – Prevents stiffness in joints and muscles. Strengthening supporting muscles – Helps maintain posture and stability. Diet & Supplements for Faster Recovery Proper nutrition is crucial for bone healing. Here are essential nutrients to include in your diet: Calcium & Vitamin D – Essential for bone regeneration. Protein – Helps rebuild muscle strength. Collagen supplements – Promotes joint and ligament healing. Conclusion Recovering from limb lengthening surgery or Height increase surgery requires dedication and patience. A carefully planned exercise regimen, combined with physiotherapy and a proper diet, ensures a successful and safe recovery. Always follow your doctor’s advice and avoidA strenuous activities until you receive medical clearance. By taking the right steps, you can regain strength and enjoy the benefits of your height transformation journey!
Limb Lengthening Surgery: How Much Height Can You Safely Gain?

Limb lengthening surgery has become a revolutionary procedure for individuals looking to increase their height. While the idea of growing taller through surgery may seem exciting, understanding the safe limits and medical aspects is crucial. In this blog, we will explore how much height you can realistically gain through limb lengthening surgery, the factors affecting the results, and the potential risks of excessive height gain. Understanding the Science Behind Limb Lengthening Limb lengthening surgery involves a procedure called distraction osteogenesis. During the surgery, the bone is carefully cut, and an external or internal fixation device gradually pulls the bone segments apart. The body naturally fills in the gap with new bone tissue, allowing for an increase in height over time. This process requires careful medical supervision and a structured recovery plan. How Much Height Can You Gain Safely? On average, most patients can safely gain between 5 cm to 8 cm (2 to 3 inches) per procedure. However, with advanced techniques, some individuals can achieve up to 15 cm (6 inches) in total by undergoing multiple surgeries. The exact height increase depends on several factors, including: Bone structure and health – Strong bones allow for better recovery and longer distraction periods. Age – Younger individuals tend to heal faster, making them ideal candidates for larger height gains. Physical fitness and muscle flexibility – More flexibility means better adaptation to lengthened bones. Doctor’s recommendation – A surgeon will determine the safest height gain limit based on medical history. Risks and Challenges of Excessive Height Gain While the possibility of gaining significant height is tempting, attempting to lengthen beyond safe limits can lead to serious complications, such as: Muscle and nerve tightness – Over-lengthening can cause muscle stiffness and nerve compression, leading to pain and mobility issues. Longer recovery time – The more bone you lengthen, the longer the healing process takes, sometimes extending beyond a year. Joint and tendon problems – Excessive lengthening may result in imbalances that affect posture and movement. Psychological stress – The long recovery period and physical changes can impact mental well-being. How to Maximize Safe and Effective Height Gain To ensure the best results while maintaining safety, follow these guidelines: Choose an experienced surgeon – Expertise plays a crucial role in minimizing risks. Stick to a structured rehabilitation plan – Physiotherapy and guided exercises are essential for mobility. Follow a nutritious diet – Calcium, vitamin D, and protein aid in bone healing and growth. Be patient and realistic – Safe height gain takes time; rushing the process can lead to complications. Conclusion Limb lengthening surgery or Height Increase Surgery offers a safe way to increase height when done within medically recommended limits. Understanding realistic expectations, following proper recovery protocols, and consulting with an expert surgeon can ensure a successful outcome. If you’re considering the procedure, consult a professional to discuss your options and set safe goals for your height enhancement journey.
Limb Lengthening Surgery | How Does It Work?
Limb lengthening surgery is a medical procedure designed to increase bone length, primarily in the legs. This surgery is commonly performed for individuals with limb length discrepancies, congenital deformities, or those seeking cosmetic height enhancement. Over the years, advancements in medical technology have made limb lengthening procedures safer and more effective. One of the leading experts in this field is Dr. Amar Sarin, a distinguished Orthopaedic Consultant specializing in Restorative and Reconstructive Surgery at Sri Balaji Action Medical Institute, New Delhi. With over 30 years of experience and 3,000+ successful surgeries, Dr. Sarin has pioneered advancements in Ilizarov surgery, Bone Transport, and Bone Remodelling. His contributions to orthopaedics, including introducing Resorbable Ankle Implants to India, have earned him significant recognition in Asia. Understanding Limb Lengthening Surgery Limb lengthening surgery involves gradual bone distraction, allowing new bone tissue to form and extend limb length. The procedure typically follows these stages: Initial Surgery – The bone (usually femur or tibia) is surgically cut (osteotomy). An external or internal device is attached to stabilize the bone. Distraction Phase – The bone segments are slowly pulled apart (about 1 mm per day), allowing new bone to grow in the gap. Consolidation Phase – The newly formed bone hardens and strengthens. Physical Therapy & Recovery – Strength-building exercises and rehabilitation ensure proper limb function and mobility. Common techniques used include the Ilizarov method (external fixator) and the Precice method (internal, motorized nail). The choice of technique depends on patient needs and the surgeon’s recommendation. Success Rate and Effectiveness Limb lengthening surgery has a high success rate, especially when performed by experienced specialists like Dr. Amar Sarin. The effectiveness of the procedure depends on: The patient’s age and bone healing capacity Adherence to post-operative care and physiotherapy Use of advanced surgical techniques (such as motorized nails, which reduce complications) On average, patients can achieve a height increase of 5-8 cm (2-3 inches) in one surgery. In some cases, multiple procedures can lead to gains of 12-15 cm (5-6 inches). Recovery Time and Post-Surgery Rehabilitation Recovery time varies based on individual healing speed and procedure type: Hospital stay: 3-5 days post-surgery Distraction phase: 2-3 months (bone lengthening at 1 mm per day) Consolidation phase: 4-6 months (bone hardening) Full recovery and normal walking: 8-12 months Physiotherapy is essential to prevent muscle stiffness, improve joint movement, and regain mobility. Potential Side Effects and Risks While limb lengthening surgery is generally safe, potential side effects include: Pain and swelling (managed with painkillers) Muscle tightness and stiffness Risk of infection (especially with external fixators) Delayed bone healing or improper alignment Nerve or blood vessel damage (rare but possible) Choosing an experienced surgeon like Dr. Amar Sarin minimizes these risks and ensures a smooth recovery process. Who Can Undergo Limb Lengthening Surgery? The ideal candidate for limb lengthening surgery: Is between 18-50 years old (younger patients heal faster) Has good bone health and overall fitness Understands the commitment required for recovery Does not have serious medical conditions affecting bone healing Consultation with an experienced orthopaedic specialist like Dr. Amar Sarin is crucial to determine eligibility. Limb Lengthening Surgery Before and After: Real Results Limb lengthening surgery has transformed the lives of many patients by enhancing their height, self-confidence, and overall quality of life. Several before-and-after case studies highlight successful height gains, functional recovery, and improved aesthetics. Dr. Amar Sarin has been featured in prominent media outlets for his remarkable work in limb lengthening and orthopaedic advancements. His patients consistently report high satisfaction rates and positive experiences. Frequently Asked Questions (FAQs) Q: What is the minimum and maximum age for limb lengthening surgery? A: The ideal age is 18-40 years, though cases beyond this range are assessed individually. Q: How painful is limb lengthening surgery? A: Pain is manageable with medications. Discomfort is highest during the distraction phase but reduces over time. Q: How many inches can you gain through height increase surgery? A: Typically, 5-8 cm (2-3 inches) per procedure, with a maximum of 15 cm (6 inches) in multiple surgeries. Q: Can both legs be lengthened at the same time? A: Yes, both legs undergo the procedure simultaneously for symmetry. Q: How long does it take to walk normally after surgery? A: Most patients regain full mobility within 8-12 months, with proper rehabilitation. Q: Are the results permanent? A: Yes, once the bone heals, the height increase is permanent. Q: Is limb lengthening surgery safe? A: When performed by skilled surgeons like Dr. Amar Sarin, the procedure is safe with minimal risks. Conclusion Limb lengthening surgery offers a life-changing opportunity for individuals looking to correct limb length discrepancies or increase their height. With advancements in surgical technology and expert care, this procedure is now safer and more effective than ever before. Choosing a highly experienced specialist like Dr. Amar Sarin ensures the best possible outcomes. With over 30 years of experience and 3,000+ successful surgeries, Dr. Sarin remains one of the most trusted names in limb lengthening and orthopaedic procedures in Asia. If you’re considering height increase surgery, consult with Dr. Amar Sarin to explore the best options for your needs and achieve safe, successful results.

