What is Limb Discrepancy? | 9 Important Facts You Must Know

What is Limb Discrepancy?: It’s a condition where one leg or arm is shorter than the other. This difference may be mild and barely noticeable, or significant enough to affect posture, gait, mobility, and overall quality of life. Limb discrepancy can develop due to birth conditions, injuries, growth issues, or diseases that affect bone health. Understanding this condition is the first step toward finding the right treatment and regaining comfort, balance, and confidence. Understanding Limb Discrepancy What Exactly Does Limb Length Discrepancy Mean? Limb discrepancy refers to unequal lengths of the limbs, most commonly the legs. When the difference is small-under 1 cm-it usually doesn’t cause major issues. But a larger discrepancy may lead to limping, joint pain, poor posture, and long-term musculoskeletal problems. Both children and adults can develop this condition, and early diagnosis plays a key role in effective management. Types of Limb Discrepancy Limb discrepancy is generally classified into: Structural (True) Discrepancy: The bones are physically shorter on one side. Functional Discrepancy: Caused by muscle imbalance, joint stiffness, or posture issues. Congenital Discrepancy: Present from birth, often due to bone growth abnormalities. Acquired Discrepancy: Develops after injury, trauma, infection, or disease. Understanding the type helps specialists plan the most suitable treatment. Causes of Limb Discrepancy Congenital Causes: Some children are born with limb differences due to conditions like: Fibular hemimelia Congenital short femur Growth plate deformities Skeletal dysplasia These disorders affect bone formation and growth patterns. Acquired Causes Limb discrepancy can also develop later in life due to: Severe fractures during childhood Bone infections such as osteomyelitis Tumors requiring bone removal Post-traumatic growth plate damage These conditions interrupt bone development, leading to uneven growth. Neuromuscular & Growth Disorders Conditions like cerebral palsy, polio sequelae, and juvenile arthritis may alter bone or muscle growth over time, resulting in noticeable limb length differences. Signs & Symptoms of Limb Discrepancy Common symptoms include: Limping or uneven walking Pelvic tilt Lower back or hip pain Early fatigue while standing or walking Uneven shoe wear Difficulty running or participating in sports Some signs are subtle in childhood but become more visible as a child grows. How Limb Discrepancy Affects Daily Life? Even small differences can impact comfort and function. Larger discrepancies may lead to: Increased stress on joints Scoliosis Poor posture Balance issues Emotional or confidence challenges Early intervention helps avoid long-term complications. Diagnosis: How Specialists Identify Limb Discrepancy Physical Examination Doctors begin by: Measuring limb length manually Assessing posture Evaluating gait Checking spine alignment This helps determine whether the discrepancy is structural or functional. Radiological Investigations Accurate bone measurements use: X-rays Scanogram CT scan for rotational deformities MRI (in rare cases) These tools help orthopedic surgeons plan precise treatments. Treatment Options for Limb Discrepancy Non-Surgical Treatments For minor discrepancies (0.5–2 cm), doctors may recommend: Shoe lifts or heel wedges Physiotherapy Monitoring every 6–12 months These solutions reduce symptoms and support natural growth in children. Surgical Treatments For larger differences, surgery is often the best solution: Epiphysiodesis: Stops the growth of the longer leg to allow the shorter leg to catch up Limb Shortening: Shortens the longer limb (rare in adults) Limb Lengthening Surgery: Gradually lengthens the shorter limb Advanced Limb Lengthening Technologies Modern techniques include: Ilizarov External Fixators LON (Lengthening Over Nail) PRECICE Magnetic Nails These allow precise, controlled bone growth with high success rates. Limb Discrepancy Treatment by Dr. Amar Sarin Dr. Amar Sarin is one of Asia’s most experienced Limb Lengthening and Limb Discrepancy correction specialists, with over 30 years of expertise and more than 3000 successful Ilizarov and reconstructive surgeries. His advanced training from Russia’s renowned Center for Reconstruction and Regeneration Surgeries and his patient-centric approach make him a trusted choice for individuals seeking safe, precise, and long-lasting correction of limb length differences. Recovery & Rehabilitation After Treatment Recovery may involve: Regular physiotherapy Gradual weight-bearing Strength and flexibility training Follow-up X-rays Use of walking aids (temporarily) Rehabilitation ensures proper bone healing and alignment. Risks, Expectations & Long-Term Results Every medical procedure carries risks such as: Infection Device-related discomfort Delayed healing Joint stiffness However, with expert surgeons and strict monitoring, limb discrepancy treatments deliver excellent long-term outcomes and significantly improve quality of life. When to Consult a Limb Lengthening Specialist? Seek medical advice if: You notice limping or gait abnormalities Your child’s one leg appears shorter You experience chronic back, hip, or knee pain There’s a sudden difference after injury A doctor recommends orthopedic evaluation Early consultation ensures timely, effective treatment. FAQs: About Limb Discrepancy Q 1. Is limb discrepancy serious? Ans: Small differences are usually harmless, but larger discrepancies can affect posture, walking, and joint health. Q 2. Can limb discrepancy correct itself in children? Ans: Mild discrepancies may improve as a child grows, but moderate to severe cases require monitoring or treatment. Q 3. What is the best treatment for limb discrepancy? Ans: It depends on the severity. Shoe lifts work for small differences, while limb lengthening surgery is recommended for large discrepancies. Q 4. Does limb discrepancy get worse over time? Ans: In growing children, discrepancies often increase with age. Early evaluation is important. Q 5. Is limb lengthening surgery safe? Ans: Yes-when performed by an experienced surgeon using modern techniques. Most patients achieve excellent outcomes. Conclusion Limb discrepancy is a manageable condition when diagnosed early and treated appropriately. From minor differences to significant limb length issues, modern orthopedic science offers safe and effective solutions to restore comfort, symmetry, and mobility. With the guidance of an expert like Dr. Amar Sarin, patients can confidently overcome challenges and achieve long-term, life-changing results. Also Read: Cross-Leg Lengthening Surgery in India – Procedure, Safety & Results Explained Femur vs Tibia Lengthening | Which Is Better for Height Increase? Shoe Lifts for Height: Benefits, Drawbacks, and Long-Term Impact How to Increase Height After 18: Foods, Supplements & Surgery Options in India Precice Cost in India | Limb Lengthening Surgery Price Explained
Cross-Leg Lengthening Surgery in India – Procedure, Safety & Results Explained
Limb lengthening surgery has evolved significantly over the last two decades. One of the most advanced and reliable methods used today in India is the Cross-Leg Lengthening Technique – a hybrid approach that offers a safer path for patients who want height gain or correction of limb deformities without relying entirely on internal devices. This method, performed by expert centres like Dr. Amar Sarin’s, combines the stability of external fixation with the precision of internal rods, giving patients faster recovery, better bone healing, and reduced complications. If you are considering limb lengthening but are confused between Precice, Ilizarov, and hybrid approaches, this guide will help you understand where Cross-Lengthening fits. What Is Cross-Leg Lengthening? Cross-Lengthening is a hybrid limb lengthening technique that uses: An external fixator (for alignment & stability) An internal nail or rod (for long-term strength & early weight-bearing) The hybrid structure allows the bone to lengthen gradually using the external fixator while the internal rod maintains alignment and protects the bone during healing. This method is particularly useful for: Patients wanting moderate height gain Patients seeking straighter legs + height gain Complex deformity correction People with lower budgets compared to Precice Those who want faster recovery than traditional Ilizarov Why Is It Called the “Cross-Leg” Technique? The name comes from the cross-support mechanism: The external fixator supports the bone from outside The internal rod supports the bone from inside Together, they “cross” in function – giving excellent stability during lengthening. How Does the Cross-Lengthening Procedure Work? 1. Pre-Surgery Planning Patients undergo: X-rays Bone density check Medical evaluation Physiotherapy assessment The surgeon also evaluates leg proportions to ensure natural, balanced outcomes. 2. Surgery & Bone Cutting (Osteotomy) A controlled cut is made in the bone (either femur or tibia). The external fixator is applied, and the internal rod is inserted. This combination reduces the risk of: Severe pain Instability Misalignment Bone collapse 3. Daily Lengthening Phase After 7-10 days of rest, lengthening begins. Daily distraction: 0.75 mm – 1 mm per day (femur) 0.5 mm – 0.75 mm per day (tibia) The external fixator gradually separates the bone, while the rod keeps it straight. 4. Consolidation Phase Once the target height is reached: The external fixator is removed first The internal rod continues to support the bone until full healing This shortens external fixator time, which is the most stressful part of Ilizarov-only methods. 5. Physiotherapy & Full Recovery Rehab includes: Range of motion exercises Strength training Ankle & knee flexibility work Gait training Most patients walk comfortably without support in 4-6 months. Who Is a Good Candidate for Cross-Lengthening? This technique is ideal for: Patients who want 7–8 cm height gain Those who want safer, faster recovery than Ilizarov-only People looking for a more affordable option than Precice Patients with bow legs, knock knees, or other deformities Individuals with mild osteoporosis or weak bone structure (the internal rod offers added support) Cross-lengthening is commonly recommended when surgeons want a balance between: Safety Affordability Stability Faster recovery How Much Height Can Cross-Lengthening Add? Femur Cross-Lengthening: 6–8 cm Tibia Cross-Lengthening: 5–6 cm In experienced hands (like Dr. Sarin’s), tibia can sometimes reach 7–8 cm, but only with excellent physiotherapy and patient compliance. Advantages of Cross-Lengthening Surgery 1. Shorter External Fixator Time Traditional Ilizarov requires 7–12 months of frame use. Cross-lengthening reduces this significantly because the internal rod carries the load after removal. 2. Better Bone Alignment & Lower Risk of Deformity The internal rod: Prevents angulation Reduces valgus/varus drift Protects against bowing during lengthening 3. Faster Rehabilitation Patients often: Start walking with support earlier Maintain better knee/ankle motion Experience fewer contractures 4. Higher Safety for Complex Cases Patients with: Bow legs Knock knees Non-union Dwarfism Congenital deformities benefit greatly from the stability of the hybrid system. Disadvantages of Cross-Lengthening Involves external fixator (though for less time) More visible scars than Precice Slightly more discomfort due to frame Risk of pin site infection (manageable with cleaning) Slower than full internal Precice method Despite these, most patients choose cross-lengthening because it offers the best balance of price, safety, and outcomes. Cross-Lengthening vs Precice vs Ilizarov Feature Cross-Lengthening Precice Ilizarov Only Comfort Moderate Very high Low External Fixator Yes (short duration) No Yes (long duration) Scarring Moderate Minimal High Safety High Very high Moderate Height Gain 6–8 cm 6–8 cm 5–7 cm Rehab Difficulty Moderate Low High Recovery Timeline Stage Time Lengthening Phase 2–3 months External Fixator Removal After height target Walk With Support 2–3 months Walk Without Support 4–6 months Full Healing 9–12 months Return to Sports 12–15 months Natural-looking gait typically returns with physiotherapy. Common Complications (and How They’re Prevented) Muscle Tightness: Regular stretching + daily physio guidance Pin Site Infection: Daily cleaning + early antibiotics Knee stiffness: Continuous range-of-motion work Ankle tightness: Especially in tibia lengthening – managed with dedicated Achilles stretching With proper rehab, most issues are reversible. Is Cross-Lengthening Safe? Yes – in experienced hands, it is extremely safe. Why? External fixator gives precise control Internal rod prevents deformity Combination reduces risk of complications seen in Ilizarov-only methods Earlier walking prevents muscle weakness This hybrid technique is especially trusted for patients traveling internationally for surgery. Why Choose Cross-Lengthening at Dr. Sarin’s Centre? 30+ years of limb reconstruction experience 3000+ successful Ilizarov & lengthening surgeries First Indian surgeon to perform live Ilizarov surgery Team specialized in deformity correction + height gain Dedicated rehab center in Gurugram Transparent pricing with no hidden charges Treated 1000+ international patients Cross-lengthening at this center is backed by some of the highest success rates in India. Conclusion: Is Cross-Leg Lengthening Right for You? Cross-Lengthening is an excellent choice for patients who want: 6–8 cm height gain Safer recovery than Ilizarov More affordable option than Precice Better bone alignment and fewer complications Reliable, proven results It offers the best middle-ground technique for height increase: not as costly as Precice, not as uncomfortable as classic Ilizarov, but combining the strengths of both. For long-term safety, balanced proportions, and predictable outcomes, cross-lengthening is one of
Femur vs Tibia Lengthening | Which Is Better for Height Increase?
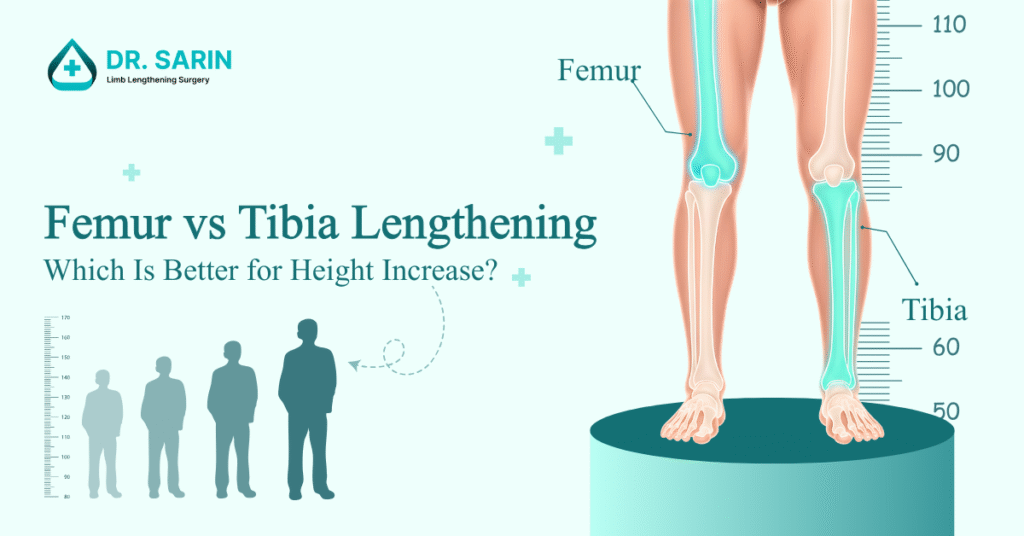
Height increase surgery has become one of the most advanced and life-changing procedures in modern orthopaedics. But one of the most common questions patients ask before planning limb lengthening is: “Which bone is better for lengthening – femur or tibia?” Both the femur (thigh bone) and tibia (shin bone) can be safely lengthened using modern techniques like Precice, Ilizarov, and Cross Lengthening. However, each bone has different biomechanics, healing patterns, comfort levels, and aesthetic outcomes. This guide will help you understand the difference between femur and tibia lengthening, how much height you can gain, recovery time, complications, and which option may suit you best. What Are the Femur and Tibia? Why Does It Matter? Femur (Thigh Bone): The strongest and longest bone in the body Surrounded by large muscle groups (quadriceps, hamstrings, gluteals) Typically allows faster healing More comfortable lengthening compared to the tibia Tibia (Shin Bone): Thinner bone with less muscle coverage More sensitive to tension Plays a major role in ankle mobility and gait More prone to stiffness during lengthening Understanding these anatomical differences helps determine the safest and most effective path for height increase. Femur Lengthening: Benefits, Limitations, and Ideal Candidates Femur lengthening is generally considered easier, faster, and more comfortable for most patients. Benefits of Femur Lengthening More Height Possible (6–8 cm safely): Most patients achieve 7–8 cm without major complications. Faster Bone Healing: Femur regenerates bone quickly due to: Rich blood supply Thick bone diameter Better muscle envelope Less Pain, Easier Physiotherapy: Femur muscles adapt better to lengthening, making rehab smoother. Natural Aesthetic Proportions: Lengthening femur creates a natural leg lengthening effect without making the shins look disproportionately long. Better for First-Time Patients: Ideal for beginners who want: Comfort Faster mobility Predictable healing Limitations of Femur Lengthening May Cause Hip Flexor Tightness: Requires stretching of: Iliopsoas Quadriceps Hamstrings Can Cause Knee Stiffness: Although usually manageable with physiotherapy. Ideal Candidates Not ideal alone for very large goals: Patients seeking 10–15 cm often combine femur + tibia (staged). Tibia Lengthening: Benefits, Limitations, and Ideal Candidates Tibia lengthening is more challenging due to the biomechanics of the ankle joint and calf muscles. Benefits of Tibia Lengthening Achieves 5–6 cm safely: Common and safe lengthening range: 5–6 cm. Experienced centers may reach 7–8 cm with strong physiotherapy (like in Dr. Sarin’s clinic). Improves Proportions in Long-Torso Patients: If someone has: Short legs Long torso: Tibia lengthening balances proportions very well. Can Correct Bow Legs or Knock-Knees Simultaneously: Especially useful for deformity corrections. Limitations of Tibia Lengthening Higher Risk of Muscle Tightness: Because heel and calf muscles shorten easily. Common issues: Achilles tendon tightness Ballerina foot (toe walking) Reduced ankle dorsiflexion More Pain During Lengthening: Due to tension in small muscles. Slower Bone Healing: Tibia has poorer blood supply. More Demanding Physiotherapy: Daily stretching of: Calf Ankle Achilles is mandatory. Femur vs Tibia Lengthening: Side-by-Side Comparison Feature Femur Lengthening Tibia Lengthening Safe Lengthening Range 6–8 cm 5–6 cm Healing Speed Faster Slower Pain Level Lower Higher Risk of Stiffness Knee stiffness Achilles & ankle tightness Rehab Difficulty Moderate High Aesthetic Impact Natural leg proportion Increases shin length Risk of Ballerina Foot Low High Recommended For Most first-time patients Short-legged patients, deformities Which Bone Gives More Height? Femur = More height per surgery: Typical: 7–8 cm Tibia = Moderate height: Typical: 5–6 cm Combined (Femur + Tibia) = Maximum height: Up to 12–15 cm over two stages. Femur or Tibia – Which Is Better for You? Here is how expert surgeons decide: Choose Femur Lengthening if you: Want easier recover Want maximum height from one surgery Have proportional legs already Are undergoing your first lengthening Choose Tibia Lengthening if you: Have short shins Want to correct bow legs or knock knees Already did femur lengthening Want balanced proportions Choose Both (Staged Sx) if you: Want 10–15 cm height Have realistic expectations Can commit to long-term physiotherapy What Do Most Patients Choose? At Dr. Sarin’s center: 70% choose femur lengthening: because it offers the best comfort and fastest recovery. 20% choose tibia lengthening: usually for bow-leg correction + height. 10% choose both staged surgeries: mainly for larger height goals (10–14 cm). How Is Femur Lengthening Performed? Options include: Precice Internal Nail Cross-Lengthening Technique Ilizarov (rarely for femur) Daily lengthening: 0.75–1 mm per day Bone fills the gap slowly and naturally. How Is Tibia Lengthening Performed? Options include: Ilizarov External Fixator (most common) Precice with STRYDE-type techniques Hybrid external+internal fixation Daily lengthening: 0.5–0.75 mm per day More conservative due to ankle tension. Recovery Time: Femur vs Tibia Stage Femur Tibia Lengthening Phase 2–3 months 2–3.5 months Bone Healing (Consolidation) 5–6 months 7–9 months Walking Without Support 4–5 months 6–7 months Return to Gym/Sports 9–12 months 12–15 months Tibia recovery is significantly longer due to ankle biomechanics. Conclusion: Femur vs Tibia – What’s the Best Choice? Both femur and tibia lengthening are effective, safe, and widely performed procedures. But they are not the same. Femur: More height, easier recovery, fewer complication Tibia: Harder, slower healing, but better for proportionality Combined: For maximum height goals For most first-time patients, Femur lengthening is the better and safer choice. You May Also Like to Know: Shoe Lift for Height: Benefits, Drawbacks, and Long Term, Impact How to Height After 18? Precice Coast in India | Limb Lenthening Surgery Price Explained How Much Height can be Increased by Surgery? Does Limb Lenthening Surgery have Any Downside?
Shoe Lifts for Height: Benefits, Drawbacks, and Long-Term Impact

Height is something many people wish they had more of. Whether for confidence, social reasons, or professional presence, appearing taller can make a difference. One of the most common short- term solutions is using shoe lift. Shoe lifts, also called height increasing insoles or heel lifts are often marketed as a simple way to look taller. They are placed inside shoes to add a few extra centimeters to a person’s height. While they may seem harmless, wearing shoe lifts regularly can negatively affect your joints, muscles, posture and psychologically. Here is a detailed look at how shoe lifts impact different parts of the body and the long-term consequences you should know While they work instantly, they also disrupt the body’s natural biomechanics. Over time, this can lead to multiple health problems. Let’s explore each one in detail. Can Shoe Lifts Cause Plantar Fasciitis or Heel Pain? Mechanism: Shoe lifts raise the heel, shifting body weight onto the back of the foot. This overstretches the plantar fascia ,the thick band of tissue that runs from the heel to the toes. Symptoms: Sharp stabbing heel pain especially in the morning or after sitting,tenderness under the arch, and swelling in severe cases. Long-term Consequence: Chronic plantar fasciitis can limit walking, sports, and daily activities. Shoe Lifts and Knee Pain: The Link Explained by Physiotherapists Mechanism: 5 cm – 8 cm of shoe lifts push the body forward, increasing the angle at which the patella (kneecap) tracks over the femur. This adds stress to the cartilage and surrounding tissues. Symptoms: Pain around or behind the kneecap, worse during stairs, squatting, or sitting for long periods. Long-term Consequence: Can progress to patellofemoral pain syndrome or early cartilage wear, raising the risk of osteoarthritis. How Shoe Lifts Can Lead to Hip Imbalance and Anterior Pelvic Tilt Mechanism: Elevating the heel tilts the pelvis forward unnaturally (anterior pelvic tilt). This shortens the hip flexors – iliopsoas, rectus femoris and weakens the gluteal muscles. Symptoms: Tight hips, reduced flexibility, aching around the hip joints, uneven walking patterns. Long-term Consequence: Chronic hip pain, imbalance between muscle groups, and inefficient gait that stresses other joints. Do Shoe Lifts Affect Posture? Understanding the Risk of Low Back Pain Mechanism: Shoe lifts elevate the heels, shifting your center of gravity forward. This can lead to an anterior pelvic tilt, increasing the curve in the lower back. This excessive arching puts strain on the lower back muscles and spine, potentially causing pain. Heel lifts can over activate anterior muscles like hip flexors and quadriceps, while weakening posterior muscles like glutes and hamstrings. This imbalance can stress the lower back, as the weakened muscles fail to support the spine properly. Symptoms: Dull aching pain in the lower back, stiffness, discomfort when standing or walking for prolong time. Long-term Consequence: Chronic low back pain, disc degeneration, and poor posture that may require rehabilitation. Heel Lifts and Achilles Tendonitis: What You Need to Know Mechanism: Since the heel is artificially elevated, the Achilles tendon which connects calf muscles to the heel bone remain in a shortened position all the time during standing ,walking and running so calf muscles and tendon do not get its natural elasticity. Over the time, reduces flexibility of tendon Achilles. Symptoms: Tight calves, heel pain at the back, tenderness along the tendon, pain during running, jumping and sport activities. Long-term Consequence: Achilles tendonitis, chronic stiffness, and even risk of tendon rupture with sudden stress. How Height Increasing Insoles Can Lead to Calf Muscle Stiffness Mechanism: Similar to the Achilles, the gastrocnemius and soleus muscles stay in a shortened position with lifts. This reduces ankle dorsiflexion range of motion. Symptoms: Cramping, fatigue, reduced ability to stretch calves fully, discomfort during sports. Long-term Consequence: Limited ankle mobility, poor athletic performance, and higher risk of injuries. How Shoe Lifts Affect Balance, Gait, and Walking Mechanics Mechanism: 1. Shoe lift changes the natural alignment of the foot, ankle, knee, hip, and spine. This shifts the body’s center of gravity forward 2. Reduced Stability: These changes make it harder for the body to maintain balance, especially on uneven ground, stairs, or when changing direction quickly. This increases the risk of tripping or falls. 3. Muscle & Joint Stress: The imbalance forces certain muscles (like calf, quadriceps, and back muscles) to overwork, which can cause fatigue, soreness, or even long-term joint strain. Symptoms: Wobbling inside shoes, ankle instability, difficulty balancing on uneven surfac. Long-term Consequences: Altered walking patterns that stress multiple joints, increasing injury risk. Psychological Effects of Wearing Shoe Lifts Daily Shoe lifts provide a quick confidence boost, but users may begin to rely on them emotionally. Without them, they may feel shorter, insecure, or anxious. Fear of social settings without lifts, low self-esteem when barefoot or in flat shoes, reduced confidence, body-image issues, and dependence on external aids instead of long-term solutions. Why This Matters Most of these issues start with mild discomfort in the feet or back but with daily, long-term use, they can lead into chronic pain, joint degeneration, and reduced mobility. Safer Use of Shoe Lifts For permanent height gain, consider medical evaluation for limb lengthening surgery FAQ: About Shoe Lifts for Height Q. If I’m considering limb lengthening surgery in future. Can I wear the shoe-lifts? Ans: If you wear shoe lifts, it can cause your iliopsoas muscles to tighten, along with ankle stiffness and calf muscle tightness. Before limb lengthening surgery, this type of muscle imbalance and stiffness is not ideal, because it can make recovery and rehabilitation more difficult. Post surgery you may developed severe hyperlodrosis and ballerina syndrome It’s better to keep your muscles flexible and well balanced before surgery. Q. Can I wear shoe lifts post limb lengthening surgery? Ans: After limb lengthening surgery, it’s not recommended to wear shoe lifts during the recovery and rehabilitation phase. Once you are fully recovered, you may wear shoe lifts occasionally if you wish. But if you are planning a second stage of limb lengthening, you should avoid
How to Increase Height After 18: Foods, Supplements & Surgery Options in India

Most teens are wondering: Can you become taller after the age of 18? Although natural growth will stop or slow down after adolescence, nutrition, posture, and bone density still play a part. Besides, limb length extension surgery is an option for a lifelong solution for those who are willing to become taller even if their growth plates closed. In the following guide, we will discuss supplements for height growth, bone supplements for health, and sophisticated Indian medical options for growth and development. Can You Actually Increase Height after 18? Role of Genetics and Growth Plates Height is quite genetically determined. Growth plates for the long bones shut up around the late teens (16-18 for females, 18-21 for males). When closed, bone growth is automatically halted. Natural Limits After Puberty When the growth plates close, natural methods (diet, exercise, supplements) can’t add inches, but they can maximize bone strength, posture, and spine alignment, making you look longer and healthier. Height Gain Supplements: Do They Actually Work? Calcium and Vitamin D These promote bone density and health. Although they don’t make you grow after the age of 18, they help inhibit bone loss and maintain your back support. Protein and Amino Acids Protein supplements (whey protein, amino acids) support muscle growth, helping spine alignment and better posture. Zinc, Magnesium, and Multivitamins Micronutrients aid bone repair, immunity, and general growth during adolescence. After the age of 18, they help the individual maintain healthy bones. Myths About Growth Pills Most online “pill for height growth” websites are dishonest. There is no pill that can re-open fused growth plates. Supplements promote bone and muscle health, not the growth of new height. Food Supplements to Increase Height Naturally Dairy, Milk, and Calcium-Rich Foods: Milk, yogurt, cheese, high in calcium and Vitamin D, both very important for bone health. Lean Protein Sources (Eggs, Chicken, Fish, Pulses): Protein develops muscles that enable proper posture and movement. Fruits and Vegetables for Bone Health: Spinach, broccoli, bananas, and oranges are rich in minerals and vitamins for bone formation. Nuts, Seeds, and Healthy Fats: Almonds and walnuts deliver the essential fatty acids and magnesium for bone strength. Lifestyle Habits That Encourage Healthy Posture and Bone Strength Exercise and Stretching: Activities like yoga, swimming, cycling, and pilates improve posture and flexibility. Sleep and Recovery: Deep sleep (7–9 hours) is essential for hormone regulation and bone repair. Posture Improvement: Upward spine, core exercises, and proper seating maximize the appearance of height. Can Surgery Increase Height After 18? Overview of Limb Lengthening Surgery Indeed, only limb lengthening surgery can make you permanently tall after the age of 18. In the surgery, the bones are slowly separated and new tissue grows automatically. Cost of Limb Lengthening Surgery in India For those seriously considering this option, here are the updated costs (including 3 months of post-surgery accommodation in a recovery facility): Precice Nail Surgery: ₹40–46 lakhs ($42,000–48,000) External Fixator (Ilizarov): ₹9–10 lakhs Cross Lengthening: ₹18–19 lakhs Why Dr. Sarin is a Credible Expert Over 30 years of experience in reconstructive and orthopedic surgery Hundreds of orthopaedic surgeons trained globally Reasonable prices compared to metro hospitals Dedicated international patient care Choosing Dr. Sarin ensures professional treatment, tested-and-proven results, and transparent pricing. FAQs on Supplements and Height Increase After 18 Q1. Can supplements increase height after 18? Ans: They can’t make you taller, but they promote bone and muscular health. Q2. Which are the top bone health supplements? Ans: Calcium, vitamin D, protein, zinc, and magnesium-containing foods. Q3. Can surgery alone increase one’s height after the age of 18? Ans: In fact, limb lengthening surgery is the only proved permanent cure. Q4. How tall can I become after surgery? Ans: Typically 6–8 cm, occasionally as large as 15 cm with repeated surgery. Q5. Limb lengthening recovery lasts for how long? Ans: Recovery lasts 9–12 months with physiotherapy. Q6. Does Dr. Sarin’s clinic cost less than other metro hospitals? Ans: Indeed, Dr. Sarin provides top-notch treatment within competitive pricing, often lower than corporate hospital rates. Conclusion: The Realistic Methods for Height Increase After Age 18 Although height increasing supplements and a healthy lifestyle support maintaining a healthy spine and good posture, supplements and lifestyle can’t add inches after growth plate closure. Limb lengthening surgery is the only definitive remedy after the age of 18. To treat the patients safely and swiftly, Dr. Sarin’s clinic at Delhi NCR offers superior limb lengthening surgery with transparent pricing and accommodation facilities for post-surgery recovery, making it a trusted choice for both Indian and international patients. You May Also Like to Know: Precice Cost in India How much Height can be Increased by Surgery Does Limb lengthening surgery have any downsides? Why do surgeons use an external fixator for limb lengthening procedures? 9 things to know before you get Leg-Lengthening Surgery
Men & Women’s Average Height In USA 2026

Average Height in USA: Gaining insight into the average height of populations can reveal important information about health, nutrition, and genetics. Let’s explore the USA average heights found in various regions of the Americas in 2026. Average Height of Latin America In Latin America, average heights vary significantly among countries due to genetic, nutritional, and socio-economic factors. Generally, Latin American countries show considerable diversity in height. Countries like Venezuela and Colombia are known for having relatively taller populations, while others like Guatemala and Honduras have shorter average heights. Average Height of North America North America is characterized by a higher average height, influenced by genetics, diet, and healthcare. Here’s a breakdown of the average heights in the United States, Canada, and Mexico: 1. United States: 2. Canada: 3. Mexico: Average Height of Central America Central America has a diverse range of heights, with some countries showing shorter averages than their northern and southern neighbors. Countries like Panama and Costa Rica are on the taller end, whereas countries like Nicaragua and Guatemala tend to have shorter average heights. Average Height of the Caribbean The Caribbean islands exhibit various heights, influenced by the region’s diverse genetic pool and nutritional standards. Countries such as Barbados, Trinidad, and Tobago have some taller averages, while others, like Haiti and the Dominican Republic, show slightly shorter averages. Also Read: Height Growth Plates: When Do Growth Plates Close? Medical Lengthening Surgical Skin Preparation for Limb Lengthening Surgery Indications for Limb Lengthening Available Methods Of Limb Lengthening
Precice Cost in India | Limb Lengthening Surgery Price Explained

For many people, increasing their height or correcting a limb length difference is a life-changing decision. With modern technology, this is now possible through advanced procedures like Precice limb lengthening surgery. But one of the first concerns patients have is: How much does Precice surgery cost in India? Let’s break it down. What is Precice Limb Lengthening? The Precice nail system is one of the most advanced methods of limb lengthening available today. Developed in the USA, it is an internal implant controlled by a magnetic remote (ERC -External Remote Controller). This allows the bone to be lengthened gradually, safely, and comfortably. Key Benefits of Precice over External Fixators: • No external frames or bulky rods • Minimal scarring for better cosmetic results • Lower risk of infection • Controlled and precise lengthening each day • Faster return to mobility and daily life For these reasons, Precice is often referred to as the gold standard for height increase surgery worldwide. Precice Cost in India In India, the average cost of Precice surgery ranges between ₹40 lakh to ₹70 lakh. The exact price depends on: Surgeon’s expertise and hospital reputation Type of Precice nail used (Precice 2 ,2.2, , etc.) Lengthening goal (usually 5–8 cm) Rehabilitation and physiotherapy requirements City and hospital facilities Comparison: In the USA or Europe, the same surgery can cost between ₹1 crore and ₹1.5 crore (USD $120,000–$180,000). This makes India an attractive and more affordable destination for patients worldwide who want height increase surgery with the same advanced technology. Why is the Cost So High? The cost of Precice surgery is largely due to: Imported Implant: The Precice nail is manufactured in the USA, making it one of the most expensive orthopedic devices in the world. Specialized Expertise: Only highly trained surgeons with years of limb reconstruction experience can safely perform this surgery. Hospital Infrastructure: World-class operating theaters, ICU support, and infection control are essential for patient safety. Rehabilitation Support: A structured physiotherapy program is necessary to regain strength and mobility. Precice Surgery with Experienced Surgeons in India India is home to some of the most experienced limb lengthening surgeons who have successfully treated patients from across the globe. For example, Dr. Amar Sarin in Delhi offers Precice limb lengthening starting at ₹46 lakh. This cost includes not only the imported implant but also expert surgical care, hospital facilities, and a dedicated rehabilitation plan. While still a significant investment, it remains far more cost effective compared to Western countries, without compromising on safety or quality. Is Precice Surgery Worth It? Choosing to undergo Precice limb lengthening in India is not just about increasing height,it’s about investing in confidence, appearance, and long term quality of life. The price may seem high at first, but when you consider the technology, safety standards, and expertise involved, it becomes clear why the cost is justified. For patients determined to change their lives through height increase surgery, India offers a balance of world-class care at nearly half the international cost. You May Also Like To Know: How Much Height can be Increased by Surgery Does Limb lengthening surgery have any downsides? Why do surgeons use an external fixator for limb lengthening procedures? 9 things to know before you get Leg-Lengthening Surgery What are the Long-Term Effects of Bone Lengthening?
How much Height can be Increased by Surgery

In today’s fast-paced world, physical appearance plays a significant role in confidence and self-esteem. This surgery has emerged as a viable option for those seeking to enhance their stature. Dr. Sarin, a renowned name in the field of cosmetic surgery, offers cutting-edge solutions for individuals aspiring to add inches to their height through surgical intervention. A Comprehensive Approach Dr. Sarin’s approach to Restorative and Reconstructive surgery is rooted in advanced medical techniques and personalized care. The procedure involves limb lengthening, a sophisticated surgical design that enables gradual, controlled extension of the bones. The Process Explained Under Dr. Sarin’s expert guidance, the height increase surgery begins with thoroughly evaluating the patient’s medical history and physical condition. This initial assessment ensures the procedure is suitable and safe for the individual. Once cleared, the surgery is conducted in a state-of-the-art facility, utilizing the latest medical equipment and techniques. During the procedure, specialized instruments make precise, controlled bone incisions. These incisions create space for the gradual lengthening process. Over time, as the bones heal, new bone tissue fills in the gaps, resulting in increased height. Personalized Care Every Step of the Way What sets Dr. Sarin apart is the emphasis on personalized care. Each patient receives a customized treatment plan tailored to their unique physiological characteristics and desired outcome. A dedicated team of medical professionals, including orthopedic surgeons and rehabilitation experts, closely monitors progress and provides guidance throughout the process. The Road to Height Enhancement: Post-Surgery Rehabilitation After the surgery, diligent post-operative care and rehabilitation are essential. Dr. Sarin’s team employs a multifaceted approach, combining physiotherapy and targeted exercises to optimize recovery and enhance the procedure’s effectiveness. Realistic Expectations and Lasting Results It’s important to note that while surgery can be a transformative experience, it’s crucial to maintain realistic expectations. Dr. Sarin ensures open and honest communication with patients, discussing achievable outcomes based on individual factors. With Dr. Sarin’s expertise and dedication to patient satisfaction, surgery becomes a safe and effective option for those looking to gain confidence through increased stature. Contact Dr. Sarin’s clinic today to journey towards a taller, more confident you. Also Read: Limb Lengthening Surgery in 2025 Limb Lengthening Surgery in India Best Diet for Bone Healing After Limb Lengthening How We Help You Return to Work and Sports After Limb Lengthening? How to Lengthen Legs Naturally & Surgically in 2025
Does Limb lengthening surgery have any downsides?

Limb lengthening surgery has gained popularity in recent years as a medical procedure that offers individuals the opportunity to enhance their height. While the desire for increased height is understandable, it’s essential to carefully consider both the advantages and potential downsides of such surgeries. On the positive side, limb lengthening surgery can be a life-changing procedure for individuals who struggle with issues related to stature. It’s particularly beneficial for those with conditions such as dwarfism or leg length discrepancies. The surgery involves carefully breaking the bone and gradually separating the segments to stimulate new bone growth. As a result, individuals can experience a noticeable increase in height. However, like any medical procedure, limb lengthening surgery is not without its drawbacks. One significant downside is the lengthy and challenging recovery process. Patients typically need to undergo a period of physical therapy and rehabilitation to regain mobility and strength. The process can be physically and emotionally demanding, requiring patience and perseverance. Another consideration is the potential for complications. While advancements in medical technology have reduced the risks, there is still a possibility of infections, nerve damage, or issues with the bone healing process. Additionally, the surgery is not always 100% effective, and the final height increase may vary from person to person. Financial considerations are also crucial. Limb lengthening surgery can be an expensive procedure, and it may not be covered by insurance in some cases. Prospective patients should carefully evaluate the cost, considering not only the surgery itself but also the associated expenses like post-operative care, rehabilitation, and follow-up appointments. Moreover, the psychological impact of limb lengthening surgery cannot be overlooked. The desire for increased height may be rooted in societal expectations and personal insecurities. It’s important for individuals considering this procedure to address the underlying reasons behind their decision and to have realistic expectations about the outcomes. In conclusion, limb lengthening surgery can be a viable option for those seeking to enhance their height, especially in cases where it addresses medical conditions. However, individuals should weigh the potential benefits against the challenges, including the demanding recovery process, potential complications, financial considerations, and the psychological impact of such a transformative procedure. As with any medical decision, individuals considering limb lengthening surgery should thoroughly weigh the benefits and potential drawbacks, consulting with Dr. Sarin to make an informed choice for their unique circumstances. Also Read: Limb Lengthening History Understanding the Phases of Limb Lengthening Bone Healing After Leg Lengthening Surgery Determining Age Limits for Leg Lengthening Surgery External Methods vs. Internal Methods of Cosmetic Leg Lengthening
Why do surgeons use an external fixator for limb lengthening procedures?

Surgeons often use an external fixator for limb lengthening procedures due to its effectiveness in gradually and precisely lengthening bones. This device consists of external metal rods, screws, and pins that are surgically attached to the bone segments on either side of the intended lengthening site. One primary reason for using an external fixator is its ability to provide controlled and gradual distraction, allowing new bone formation to occur in the gap created. By making tiny adjustments to the fixator, surgeons can regulate the rate of bone distraction, minimizing complications and maximizing the body’s natural healing process. Another advantage is its versatility and adaptability. Surgeons can customize the fixator’s configuration to suit the patient’s needs and the targeted bone for lengthening. Additionally, the external nature of the fixator simplifies wound care and reduces the risk of infections compared to internal devices. The external fixator also permits early weight-bearing and mobility, promoting quicker recovery and rehabilitation for the patient. This aspect contributes significantly to a patient’s quality of life during the lengthening process. Overall, using an external fixator in limb lengthening surgery offers precise control, adaptability, reduced infection risk, and enhanced patient mobility, making it a preferred choice for many surgeons. Also Read: Reasons Why People Get Cosmetic Leg-Lengthening Surgery Done Does Limb lengthening surgery have any downsides? Limb Lengthening History Understanding the Phases of Limb Lengthening Bone Healing After Leg Lengthening Surgery
