ACL Surgery

Anterior Cruciate Ligament (ACL) surgery is a common procedure performed to repair or reconstruct a torn ACL, one of the major ligaments in the knee. ACL injuries often occur due to sudden changes in direction, awkward landings, or direct trauma, making them prevalent in sports such as soccer, basketball, and skiing. The goal of ACL surgery is to restore stability, range of motion, and function to the knee, enabling patients to return to their daily activities or sports. Depending on the severity of the injury, ACL surgery may involve repairing the ligament or reconstructing it using a graft from another part of the body. Nonsurgical Treatment In some cases, nonsurgical treatment can be an effective way to manage an ACL injury. This approach is typically recommended for patients with partial tears or less physically demanding lifestyles. Nonsurgical treatments focus on rehabilitating the knee through physical therapy and targeted exercises to improve strength, flexibility, and balance. Bracing is often used to provide additional knee support during recovery. Pain management techniques, such as anti-inflammatory medications and ice therapy, can also be helpful in reducing discomfort and swelling. Patients with less active lifestyles or those who do not engage in high-impact sports may find nonsurgical treatments sufficient to manage their symptoms and prevent further damage. However, for individuals looking to return to an active lifestyle, nonsurgical treatments may not fully restore knee stability, making surgical intervention necessary. Surgical Treatment and ACL Reconstruction For those with complete ACL tears or who are highly active, surgical treatment becomes the best option. ACL reconstruction is the most common surgical approach and involves replacing the damaged ligament with a tissue graft. This graft is often taken from the patient’s own body, typically from the patellar tendon, hamstring, or quadriceps tendon. In some cases, a cadaver graft may be used. The surgery is usually performed arthroscopically, meaning small incisions are made, and specialized tools and cameras are used to perform the procedure. This minimally invasive technique reduces the recovery time and the risk of complications. During the surgery, the torn ACL is removed, and the graft is positioned and secured in place. Over time, the body integrates the graft, and it functions like a natural ACL. How Long Does Rehabilitation Take After Surgery? Rehabilitation is a critical part of the recovery process after ACL surgery. While the surgical procedure repairs the ligament, rehabilitation focuses on restoring strength, flexibility, and range of motion to the knee. The length of rehabilitation varies depending on the individual and the severity of the injury but typically lasts between six to nine months. In the initial weeks following surgery, patients work on managing pain, reducing swelling, and regaining the ability to walk. Gradually, they progress to exercises that strengthen the quadriceps and hamstrings, improve balance, and increase the knee’s range of motion. Physical therapy is often recommended to guide patients through these exercises and ensure proper technique. For athletes, returning to sports can take anywhere from six to twelve months, depending on their progress and the nature of the sport. It’s essential to follow the rehabilitation plan closely to prevent re-injury and ensure long-term success. What Are the Potential Complications After Surgery? While ACL surgery is generally safe and effective, like any surgical procedure, it carries potential risks. Some common complications include: Infection: Although rare, infections can occur at the surgical site. Proper post-operative care, including cleaning the incision area, reduces this risk. Blood Clots: There is a small risk of developing blood clots after surgery, particularly in the leg veins. Patients are often advised to stay active and use compression devices to prevent clot formation. Knee Stiffness or Loss of Motion: Some patients may experience difficulty regaining full range of motion, especially if rehabilitation is delayed or inadequate. Graft Failure: In rare cases, the graft used for ACL reconstruction may not integrate properly, or it may stretch or tear, leading to the need for revision surgery. Chronic Pain: Some patients report ongoing pain or discomfort after surgery, although this is less common. Overall, ACL surgery has a high success rate, particularly when followed by a structured rehabilitation program. Most patients are able to return to their normal activities or even sports, though full recovery may take time.
Hip Replacement Surgery
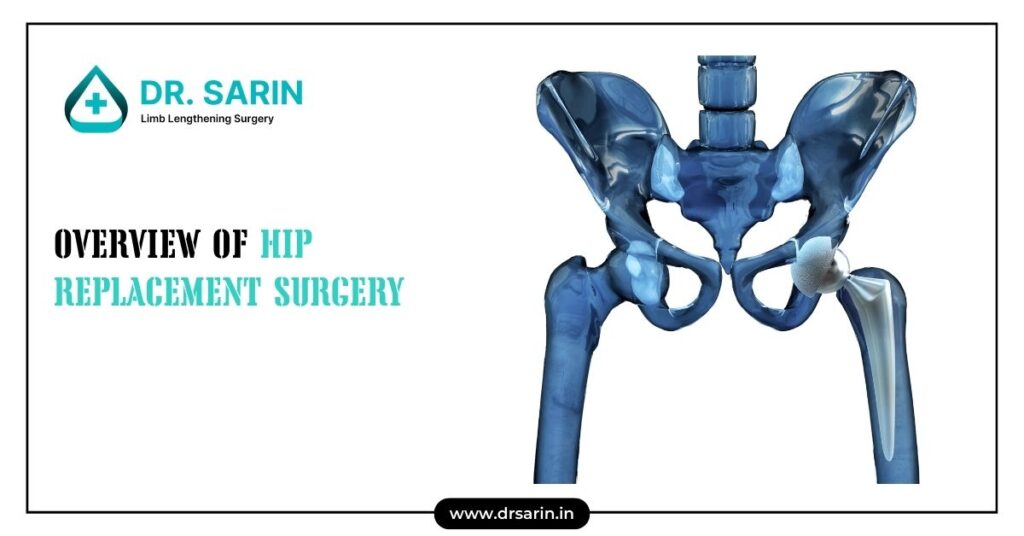
Hip replacement surgery, also known as hip arthroplasty, is a common procedure aimed at relieving hip pain and improving joint function. This surgery involves removing the damaged sections of the hip joint and replacing them with artificial components, typically made from metal, plastic, or ceramic materials. Hip replacement is generally considered for individuals suffering from severe arthritis, hip fractures, or other degenerative joint conditions that affect their mobility and quality of life. By restoring the function of the hip joint, this surgery can allow patients to return to their everyday activities and significantly reduce their pain levels. There are two primary types of hip replacement surgeries: total hip replacement (THR) and partial hip replacement. In a total hip replacement, both the ball (femoral head) and the socket (acetabulum) of the hip joint are replaced. Partial hip replacement typically involves replacing only the femoral head. The choice between these procedures depends on the extent of damage to the hip joint, the patient’s age, overall health, and activity level. Why is Hip Replacement Surgery Needed? Hip replacement surgery is typically recommended for individuals who experience chronic hip pain and limited mobility that doesn’t improve with non-surgical treatments such as physical therapy, medications, or injections. The most common reason for needing hip replacement is osteoarthritis, a degenerative joint disease that wears down the cartilage between bones, leading to pain and stiffness. Other conditions that may necessitate hip replacement include rheumatoid arthritis, hip fractures, avascular necrosis (a condition where the blood supply to the bone is reduced, causing the bone to die), and developmental hip dysplasia. For many patients, hip pain can significantly interfere with daily activities such as walking, climbing stairs, and even resting. When hip joint deterioration begins to affect sleep, work, or basic movements, hip replacement surgery can offer a long-term solution. The surgery is designed to alleviate pain, restore range of motion, and improve overall function, allowing patients to lead a more active lifestyle. Preparing for Hip Replacement Surgery Preparation is a key factor in ensuring a successful hip replacement surgery and smooth recovery. Before the surgery, patients will undergo a thorough medical evaluation, which includes blood tests, X-rays, and a physical examination to ensure they are fit for the procedure. The surgeon may also suggest losing weight, quitting smoking, or engaging in a preoperative exercise regimen to improve overall health and muscle strength. This preparation can help to optimize the outcome of the surgery. Patients should inform their medical team of any medications they are taking, as some drugs may need to be paused or adjusted before the surgery. Additionally, preparing the home environment for post-surgery recovery is important. Patients may need to arrange for assistive devices such as crutches, walkers, or grab bars in the bathroom. It’s also advisable to have a support system in place, as some assistance will be required for daily tasks during the initial recovery period. What to Expect During Hip Replacement Surgery During hip replacement surgery, patients are typically placed under general anesthesia, though in some cases, spinal or epidural anesthesia may be used. The surgery usually takes about 1-2 hours. In a standard procedure, the surgeon makes an incision over the hip and carefully removes the damaged bone and cartilage. The artificial joint components (prostheses) are then inserted to replicate the movement of a healthy hip joint. Depending on the type of surgery and the surgeon’s preference, either cemented or uncemented prosthetics may be used. Minimally invasive techniques, which involve smaller incisions and less muscle disruption, have become more common and may result in quicker recovery times. After the surgery, patients will be moved to a recovery room where their vital signs are monitored. Most patients stay in the hospital for 1-3 days, but the recovery time varies depending on the individual’s overall health and the complexity of the surgery. In the days following surgery, physical therapy will begin to help patients regain strength and mobility. Although full recovery can take several months, most patients experience significant pain relief and improved joint function within a few weeks of surgery. With proper care, a hip replacement can last 15-20 years, allowing individuals to enjoy a better quality of life for years to come.
Factors That Can Influence the Price of Limb Lengthening Surgery in India

Limb lengthening surgery is a complex procedure that involves the gradual extension of bones to correct discrepancies or enhance height. In India, the cost of this surgery can vary significantly due to several factors. Understanding these factors can help patients and their families make informed decisions when planning for the procedure. Here’s a breakdown of the key elements that can influence the price of limb lengthening surgery in India. Hospital Reputation and Infrastructure The reputation and infrastructure of the hospital where the surgery is performed are major factors influencing the cost. Hospitals with advanced technology, state-of-the-art equipment, and a strong track record of successful outcomes tend to charge higher fees. Moreover, well-established hospitals often provide better post-operative care, which is crucial for a procedure as delicate as limb lengthening. The Expertise and Experience of Medical Professionals The surgeon’s expertise and experience are critical determinants of the surgery’s cost. Surgeons with extensive experience and specialization in limb lengthening procedures often charge higher fees due to their proven track record and the complexity of the surgery. Additionally, the involvement of a skilled surgical team, including anesthetists and physiotherapists, also adds to the overall cost. The Type and Frequency of Diagnostic Procedures Before the surgery, patients undergo various diagnostic tests such as X-rays, MRIs, and blood tests to assess their suitability for the procedure and plan the surgery. The type and frequency of these diagnostic procedures can significantly impact the overall cost. Advanced imaging techniques or repeated tests to monitor progress during the treatment phase can increase expenses. The Choice of Treatment Modality Limb lengthening can be performed using different techniques, such as the Ilizarov method, intramedullary nails, or external fixators. The choice of treatment modality greatly affects the cost of the surgery. Some methods require more advanced equipment and longer hospital stays, which can drive up the price. The complexity of the chosen technique also influences the length of recovery and the need for follow-up procedures, adding to the overall cost. Medication Costs Medication is an essential part of the limb lengthening process, both pre- and post-surgery. The cost of pain management, antibiotics, and other necessary drugs can vary depending on the brand, dosage, and duration of treatment. High-quality medications, often prescribed to ensure a smoother recovery and minimize the risk of complications, can increase the overall cost of the surgery. Duration of Treatment The duration of the treatment process, which includes both the surgery and the post-operative recovery period, can affect the overall cost. Limb lengthening is a gradual process that can take several months to complete, especially during the bone consolidation phase. Prolonged treatment may lead to additional hospital visits, follow-up consultations, and extended use of medical devices, all contributing to higher expenses. Geographical Location The geographical location of the hospital also plays a significant role in determining the cost of limb lengthening surgery. Hospitals in metropolitan cities like Delhi, Mumbai, or Bangalore tend to charge more due to higher operational costs, demand for specialized medical services, and access to advanced technology. In contrast, hospitals in smaller cities or towns might offer the procedure at a lower cost, albeit with potentially limited resources or less experienced medical professionals. Hospitalization Expenses Hospitalization expenses, including room charges, nursing care, and other in-hospital services, can add substantially to the overall cost of the surgery. Private rooms, luxury amenities, and extended stays can significantly increase hospitalization costs. Patients should consider these factors when choosing their hospital, as a comfortable and supportive environment is essential for recovery but can also raise the cost. Government Policies and Subsidies Government policies and subsidies can sometimes influence the cost of limb lengthening surgery in India. In some cases, government hospitals or schemes may offer the surgery at a subsidized rate for eligible patients. However, these options might come with longer waiting periods or limited access to advanced treatment modalities. Understanding available government support can help in reducing the financial burden of the surgery. Medical Tourism Packages India is a popular destination for medical tourism, and many hospitals offer comprehensive packages that include surgery, accommodation, transportation, and post-operative care. These packages can be cost-effective for international patients seeking high-quality medical care at a lower cost compared to their home countries. However, the overall price of such packages can vary based on the inclusions, the hospital’s reputation, and the level of care provided. When considering limb lengthening surgery in India, it’s essential to take into account these various factors that can influence the overall cost. By carefully evaluating the hospital, medical professionals, treatment modalities, and additional expenses, patients can make informed decisions that align with their budget and healthcare needs.
Hemihyperplasia

Hemihyperplasia, also known as hemihypertrophy, is a rare congenital condition characterized by the asymmetric growth of one side of the body. In this disorder, one side (either the left or right) of the body grows larger than the other, leading to noticeable differences in limb length, facial asymmetry, and body size. Hemihyperplasia can affect a specific part of the body, such as a limb, or it can extend to multiple areas, including the face, torso, and organs. The cause of hemihyperplasia is often linked to genetic mutations, although the exact mechanism is not fully understood. It may occur sporadically or as part of syndromes such as Beckwith-Wiedemann syndrome (BWS) and Proteus syndrome. Hemihyperplasia is significant because it increases the risk of certain tumors, particularly in childhood. Early detection and ongoing medical monitoring are crucial for individuals with this condition. Symptoms The symptoms of hemihyperplasia can vary widely depending on the severity of the asymmetry and the areas of the body involved. Common signs include: Asymmetrical Growth: One side of the body, including limbs, hands, feet, or facial features, grows larger or longer than the other. Facial Differences: Visible differences in facial structure, including uneven cheeks, eyes, or jawline. Limb Length Discrepancy: A noticeable difference in the length of arms or legs, which can lead to gait problems or scoliosis. Skin Differences: Changes in skin color or texture on the larger side of the body. Organ Asymmetry: Enlargement of organs such as the kidneys or liver on one side of the body, though this is less common. The condition is usually present at birth or becomes apparent during early childhood. Parents and healthcare providers may notice that one side of the child’s body grows at a faster rate, prompting further evaluation. Diagnosis Diagnosing hemihyperplasia involves a combination of clinical evaluation, imaging studies, and genetic testing. The diagnostic process typically includes: Physical Examination: A thorough assessment of the child’s growth patterns, including measuring limb length and observing facial asymmetry. Imaging Studies: X-rays, ultrasound, MRI, or CT scans may be used to evaluate internal organs, bones, and tissues, as well as monitor any associated risks like tumors. Genetic Testing: Genetic analysis is crucial to identify underlying mutations or syndromes associated with hemihyperplasia, such as Beckwith-Wiedemann syndrome. Identifying these conditions helps guide long-term management and surveillance. Early diagnosis is critical not only for addressing cosmetic and functional issues but also for monitoring the increased risk of developing certain tumors, such as Wilms tumor, a kidney cancer commonly associated with hemihyperplasia. Treatment The treatment of hemihyperplasia depends on the specific symptoms and complications the individual faces. Options may include: Surveillance for Tumors: Due to the elevated cancer risk, especially in childhood, regular abdominal ultrasounds and blood tests (for alpha-fetoprotein levels) are often recommended. Monitoring typically continues until around age 8, when the risk decreases. Orthopedic Interventions: Limb length discrepancies can be managed through orthotic devices, shoe lifts, or, in severe cases, surgery such as limb lengthening or epiphysiodesis (a procedure to halt growth in the longer limb). Cosmetic and Reconstructive Surgery: For facial asymmetry or other noticeable differences, plastic surgery may be considered to improve appearance and function. Physical and Occupational Therapy: These therapies can help manage gait abnormalities, muscle imbalances, and improve coordination. Genetic Counseling: Families may benefit from genetic counseling to understand the condition and its implications, particularly if hemihyperplasia is linked to a genetic syndrome. While there is no cure for hemihyperplasia, early detection and a multidisciplinary treatment approach can help manage symptoms, improve quality of life, and reduce the risk of complications.
Legg-Calve-Perthes disease
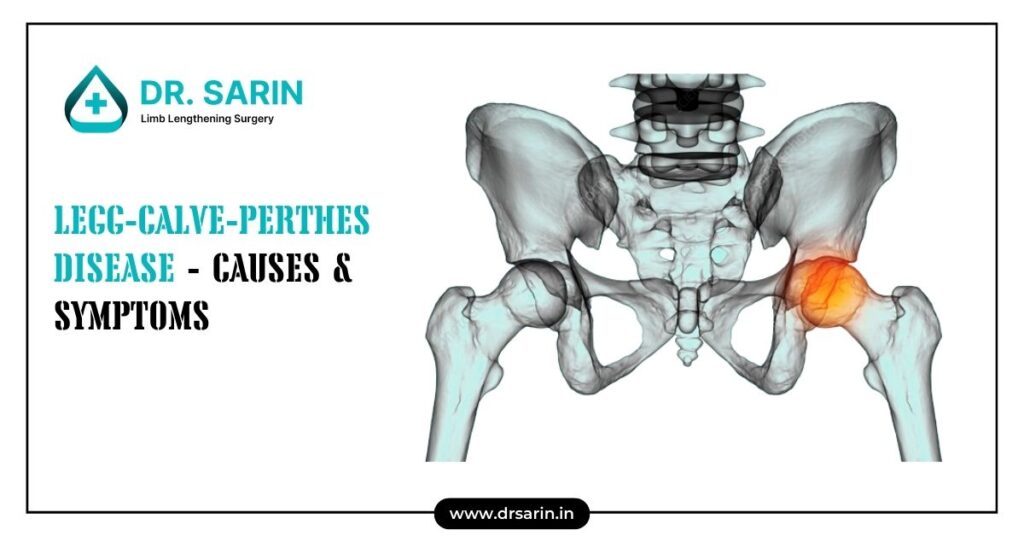
Legg-Calvé-Perthes disease is a rare childhood condition that affects the hip joint, leading to the gradual breakdown of the femoral head (the ball of the hip joint). The disease occurs when there is a temporary loss of blood supply to the rounded head of the femur, causing the bone tissue to weaken and die. As the bone loses its strength, it can become flattened or misshapen, leading to hip joint instability and potential long-term complications if untreated. The condition typically affects children between the ages of 4 and 10 and is more common in boys than girls. Early diagnosis and treatment are crucial for preventing lasting damage and promoting proper bone regrowth. Symptoms The symptoms of Legg-Calvé-Perthes disease can vary depending on the stage of the condition and the extent of damage to the femoral head. Common signs and symptoms include: Limping: A child may develop a noticeable limp, often without any known cause or injury. Hip, Groin, or Knee Pain: Pain is usually felt in the hip area but can also radiate to the groin, thigh, or knee. Limited Range of Motion: The child may have difficulty moving the hip joint fully, especially during activities like walking, running, or climbing stairs. Stiffness and Weakness: The hip may feel stiff, and the muscles around the hip joint can weaken over time. Shortened Leg: In advanced cases, one leg may appear shorter than the other due to changes in bone structure. When to See a Doctor It is important to consult a healthcare provider if your child shows signs of persistent limping, complains of hip, groin, or knee pain, or exhibits a reduced range of motion in the hip. Early intervention is key to managing Legg-Calvé-Perthes disease effectively. Prompt medical attention can help prevent severe complications and ensure the best possible outcome for your child. Causes The exact cause of Legg-Calvé-Perthes disease remains unclear. However, it is believed to result from a disruption in the blood flow to the femoral head. Without sufficient blood supply, the bone begins to die and gradually collapses. Over time, the blood supply usually returns, and the bone heals, but the shape of the femoral head may be permanently altered. Factors that may increase the risk of developing the condition include genetics, environmental factors, and certain clotting disorders. Although it is more common in boys, girls who develop the disease often have more severe symptoms. Complications If left untreated, Legg-Calvé-Perthes disease can lead to significant complications, such as: Hip Joint Deformity: As the bone heals, it may not regain its round shape, leading to a misshapen femoral head that doesn’t fit properly in the hip socket. Early-Onset Arthritis: Irregularities in the hip joint can lead to wear and tear over time, increasing the risk of developing osteoarthritis at an early age. Chronic Pain and Stiffness: Even after the bone heals, some children may continue to experience pain, stiffness, and limited mobility in the hip. Leg Length Discrepancy: Significant damage to the femoral head can cause one leg to be shorter than the other, potentially requiring corrective surgery. Early detection and appropriate treatment are critical for minimizing complications. Treatment options may include physical therapy, bracing, and in some cases, surgical intervention to restore joint function and improve long-term outcomes.
Skeletal Dysplasia

Skeletal dysplasia is a group of rare genetic disorders that affect the development and growth of bones and cartilage, leading to abnormalities in the size and shape of the limbs, spine, and other skeletal structures. These disorders, often referred to as dwarfism or short stature conditions, can vary widely in severity, from mild cases that result in short stature with few complications, to more severe forms that can cause significant physical and functional impairments. Skeletal dysplasia affects people from all racial and ethnic backgrounds and can manifest at any stage of development, from prenatal life through adulthood. The condition is caused by mutations in various genes that regulate bone and cartilage development, leading to a wide range of clinical presentations. What are the Types of Skeletal Dysplasia? There are over 400 different types of skeletal dysplasia, each with its unique characteristics and genetic causes. The most common and well-known types include: Achondroplasia: This is the most common form of dwarfism, characterized by short stature, with disproportionately short arms and legs, a large head, and a prominent forehead. Achondroplasia is caused by mutations in the FGFR3 gene. Thanatophoric Dysplasia: This is a severe form of skeletal dysplasia that is often fatal in infancy. It is characterized by extremely short limbs, narrow chest, and a small ribcage that can lead to respiratory insufficiency. It is also caused by mutations in the FGFR3 gene. Osteogenesis Imperfecta: Also known as brittle bone disease, this group of disorders is characterized by fragile bones that break easily, often with little or no apparent cause. The severity of osteogenesis imperfecta can vary widely, from mild cases with only a few fractures to severe cases with multiple fractures and bone deformities. Multiple Epiphyseal Dysplasia: This condition affects the growth of the long bones, leading to short stature, joint pain, and early onset arthritis. It is caused by mutations in several different genes that are involved in cartilage and bone formation. Diastrophic Dysplasia: This type of skeletal dysplasia is characterized by short stature, joint contractures, and deformities of the hands and feet. It can also lead to spinal deformities such as scoliosis. Symptoms and Causes The symptoms of skeletal dysplasia can vary widely depending on the specific type and severity of the condition. Common symptoms may include: Short stature: Most forms of skeletal dysplasia result in short stature, which may be disproportionate, with shorter limbs compared to the trunk. Abnormal bone growth: Irregularities in bone development can lead to deformities such as bowing of the legs, curvature of the spine (scoliosis or kyphosis), and a large head with a prominent forehead. Joint problems: Many individuals with skeletal dysplasia experience joint pain, stiffness, or limited range of motion due to abnormal joint development. Respiratory issues: Some forms of skeletal dysplasia, particularly those affecting the chest and ribcage, can lead to respiratory difficulties. Hearing loss: Certain types of skeletal dysplasia can cause conductive hearing loss due to abnormalities in the bones of the middle ear. The causes of skeletal dysplasia are primarily genetic. Mutations in specific genes that regulate bone and cartilage growth are responsible for these conditions. Some cases are inherited in an autosomal dominant or recessive manner, while others may result from spontaneous mutations that occur for the first time in the affected individual. Diagnosis and Treatments Diagnosing skeletal dysplasia typically involves a combination of clinical examination, imaging studies, and genetic testing. Prenatal ultrasound can sometimes detect signs of skeletal dysplasia before birth, especially in more severe cases. After birth, X-rays and other imaging techniques, such as MRI or CT scans, are used to assess bone abnormalities. Genetic testing is crucial for confirming the specific type of skeletal dysplasia and understanding the underlying genetic mutations. Treatment for skeletal dysplasia depends on the specific type and severity of the condition. While there is no cure for skeletal dysplasia, various interventions can help manage symptoms and improve quality of life. These may include: Orthopedic surgery: In some cases, surgery may be needed to correct bone deformities, stabilize joints, or address spinal issues such as scoliosis. Physical therapy: Physical therapy can help improve mobility, strengthen muscles, and reduce joint pain. Pain management: Medications or other therapies may be used to manage chronic pain associated with joint or bone abnormalities. Hearing aids: For individuals with hearing loss due to skeletal dysplasia, hearing aids or other assistive devices may be beneficial. Respiratory support: In cases where skeletal dysplasia affects the ribcage and breathing, respiratory support, such as ventilators or CPAP machines, may be necessary. In conclusion, skeletal dysplasia is a complex group of genetic disorders that require a multidisciplinary approach to diagnosis and management. Early detection and intervention can significantly improve outcomes, allowing individuals with skeletal dysplasia to lead fulfilling lives despite the challenges posed by their condition.
Overview of Knee Replacement Surgery

Knee replacement surgery, also known as knee arthroplasty, is a common medical procedure designed to replace the weight-bearing surfaces of the knee joint to relieve pain and disability. It is often recommended for patients suffering from severe knee arthritis, particularly osteoarthritis, rheumatoid arthritis, or post-traumatic arthritis. During the surgery, the damaged or worn-out parts of the knee are removed and replaced with artificial components made of metal and plastic. The aim is to restore the function of the knee, improve mobility, and reduce pain, enabling patients to return to their daily activities with greater ease. This surgery has become increasingly popular and effective over the years, with advancements in surgical techniques and implant technology contributing to better outcomes and quicker recovery times. However, as with any major surgical procedure, it’s essential for patients to understand the reasons behind the surgery, the potential risks, how to prepare, and what to expect during and after the procedure. Why It’s Done Knee surgery is primarily done to relieve severe pain and disability caused by damaged knee joints. It is often considered when other treatments such as medication, physical therapy, or less invasive surgeries have failed to provide adequate relief. The most common reasons for needing knee replacement surgery include: Osteoarthritis: A degenerative joint disease that typically affects older adults, leading to the breakdown of joint cartilage and underlying bone. Rheumatoid Arthritis: An autoimmune condition that causes chronic inflammation in the joints, leading to pain and joint damage. Post-Traumatic Arthritis: Arthritis that occurs after a serious knee injury, which may result in long-term damage to the knee joint. Knee Deformities: Conditions like bowed legs or knock knees that can lead to uneven pressure on the knee joint, causing wear and tear over time. Total Knee Replacement is usually recommended when the pain becomes so severe that it interferes with daily activities such as walking, climbing stairs, or even sitting and standing. The surgery can significantly improve the quality of life for those who suffer from chronic knee pain and limited mobility. Risks While knee replacement surgery is generally safe, it does carry some risks, as with any major surgery. Understanding these risks is crucial for making an informed decision. Some of the potential risks include: Infection: Although rare, infections can occur at the surgical site or within the knee joint. This may require additional treatment or even a second surgery. Blood Clots: After surgery, there is a risk of developing blood clots in the veins of the legs, which can be dangerous if they travel to the lungs. Implant Problems: Over time, the artificial knee joint may wear out, loosen, or dislocate, potentially requiring revision surgery. Nerve Damage: There is a small risk of damage to the nerves surrounding the knee, which can lead to numbness, tingling, or weakness. Stiffness: Some patients may experience stiffness in the knee after surgery, which can limit mobility. It’s important to discuss these risks with your surgeon and weigh them against the potential benefits of the surgery. How You Prepare Proper preparation before knee surgery can significantly impact the success of the procedure and your recovery. Here are some steps to take: Medical Evaluation: Your doctor will conduct a thorough medical evaluation, including blood tests, imaging studies, and a review of your medical history. Pre-Surgery Exercises: Engaging in strengthening exercises for the knee and surrounding muscles can help improve your recovery. Home Preparation: Arrange your home to accommodate your post-surgery needs. This may include installing safety bars, securing a comfortable place to rest, and preparing for limited mobility. Medications: Discuss your current medications with your doctor, as some may need to be adjusted or stopped before surgery. What You Can Expect During the Procedure Knee replacement surgery typically takes one to two hours. You will be given anesthesia to ensure you are comfortable throughout the procedure. The surgeon will make an incision over the knee to access the joint, remove the damaged bone and cartilage, and then replace them with the artificial joint components. The new knee joint will be tested for proper alignment and function before the incision is closed. After the Procedure After surgery, you will be taken to a recovery room where your vital signs will be closely monitored. Pain management is an essential part of the recovery process, and you will be given medications to control pain. Physical therapy will begin as soon as possible, often within 24 hours after surgery. The goal is to gradually restore movement and strengthen the muscles around the new joint. Most patients stay in the hospital for a few days before being discharged to continue their recovery at home or in a rehabilitation facility. Full recovery can take several weeks to months, depending on your overall health and adherence to the prescribed rehabilitation plan.
Difference in Upper Extremity Limb Length

The upper extremity, comprising the arm, forearm, and hand, is a complex structure that facilitates a wide range of motions and functions. The skeletal anatomy includes the humerus, radius, and ulna, which are supported by a network of muscles, tendons, ligaments, and nerves. Proper alignment and length of these bones are crucial for optimal function and symmetry. Description Upper extremity limb length discrepancy (UELLD) refers to a condition where there is a noticeable difference in the length of the arms. This disparity can impact both cosmetic appearance and functional abilities, leading to challenges in performing daily activities. The discrepancy may be mild or severe, and its impact on the individual can vary widely. Accurate diagnosis and appropriate treatment are essential for managing the condition effectively. Cause Congenital Upper Limb Length Discrepancy Congenital UELLD is present at birth and can result from a variety of factors, including genetic mutations, developmental disturbances, or conditions affecting fetal growth. Common congenital conditions associated with UELLD include: Fibular Hemimelia: A rare congenital condition where part or all of the fibula bone is missing. Amniotic Band Syndrome: A condition caused by entanglement of the fetal limbs in fibrous amniotic bands, leading to restricted growth and development. Radial Club Hand: A condition characterized by the underdevelopment or absence of the radius bone, resulting in a shorter forearm. Congenital UELLD is often detected early in life, allowing for timely intervention and management. Acquired Limb Length Discrepancy Acquired UELLD develops after birth due to various factors, such as trauma, infection, or medical conditions. Common causes include: Trauma: Fractures or injuries to the growth plates in children can disrupt normal bone growth, leading to length discrepancies. Severe fractures may require surgical intervention to restore limb length and function. Infections: Bone infections (osteomyelitis) can damage growth plates or bone tissue, leading to discrepancies in limb length. Tumors: Both benign and malignant bone tumors can affect bone growth and development, resulting in length discrepancies. Neurological Conditions: Conditions like cerebral palsy can lead to muscle imbalances and skeletal deformities, contributing to UELLD. Symptoms The symptoms of UELLD can vary based on the severity of the discrepancy and the underlying cause. Common symptoms include: Visible Difference in Arm Length: One arm may appear noticeably shorter or longer than the other. Functional Limitations: Difficulty in performing tasks that require symmetrical arm movement, such as lifting, carrying, or reaching. Musculoskeletal Pain: Discrepancies in limb length can lead to compensatory movements and postural imbalances, causing pain in the shoulders, back, or neck. Asymmetrical Muscle Development: The shorter limb may develop differently in terms of muscle mass and strength compared to the longer limb. Psychosocial Impact: Visible limb length discrepancies can affect self-esteem and body image, particularly in children and adolescents. Diagnosis and Treatment Diagnosis of UELLD typically involves a thorough clinical examination, medical history review, and imaging studies such as X-rays or MRI scans to determine the extent and cause of the discrepancy. Treatment options depend on the severity of the condition and may include: Non-Surgical Management: For mild discrepancies, non-surgical approaches such as physical therapy, orthotics, and shoe lifts can help manage symptoms and improve function. Surgical Intervention: In cases of severe UELLD, surgical procedures like limb lengthening, bone grafting, or corrective osteotomies may be necessary to restore symmetry and function. Early diagnosis and intervention are crucial in managing UELLD effectively, minimizing complications, and improving the quality of life for affected individuals.
What are the symptoms of Limb Lengthening?
Limb lengthening is a complex medical procedure used to increase the length of bones, typically performed to address discrepancies in limb length or to enhance overall limb functionality. Understanding the symptoms associated with this procedure can help individuals prepare for the process and manage their recovery effectively. Here’s a look at some common symptoms and issues experienced during and after limb lengthening: 1. A Leg Shorter Than the Other One of the primary reasons for undergoing limb lengthening surgery is to address differences in leg length. Initially, after the surgery, there may be a noticeable difference in leg lengths as the procedure progresses. Symptoms: Management: 2. Walking Issues After limb lengthening surgery, patients often experience difficulties with walking due to changes in limb length and adjustments required by the body. Symptoms: Management: 3. Posture Issues Changes in limb length can affect posture, as the body must adjust to new proportions. This adjustment can lead to various postural issues. Symptoms: Management: 4. Pain Pain is a common symptom associated with limb lengthening surgery, as the procedure involves significant adjustments to the bones and surrounding tissues. Symptoms: Management: Conclusion The symptoms associated with limb lengthening can vary, but they generally include differences in leg length, walking difficulties, posture issues, and pain. Proper management and a comprehensive approach to rehabilitation and support can help address these symptoms and ensure a smoother recovery process. If you are considering limb lengthening surgery, it’s essential to consult with a qualified healthcare professional to discuss potential symptoms and develop a personalized plan for managing them effectively.
Achondroplasia

Achondroplasia is a common cause of dwarfism, characterized by specific physical features and medical conditions. Understanding this genetic disorder is crucial for providing appropriate care and support to affected individuals and their families. This article overviews achondroplasia, its causes, symptoms, diagnosis, treatment, and more. What is Achondroplasia? Achondroplasia is a genetic disorder that affects bone growth, leading to dwarfism. Individuals with achondroplasia have a normal-sized torso but shorter limbs, particularly the upper arms and thighs. The condition results from mutations in the FGFR3 gene regulating bone growth. What is the Difference Between Achondroplasia and Skeletal Dysplasia (Dwarfism)? Skeletal dysplasia is characterized by abnormal bone growth and development, leading to short stature. Achondroplasia is the most common type of skeletal dysplasia. While all individuals with achondroplasia have skeletal dysplasia, not all skeletal dysplasia cases are achondroplasia. Is Achondroplasia Hereditary? Achondroplasia is usually inherited in an autosomal dominant manner, meaning only one copy of the mutated gene is required for the condition to develop. However, most cases (about 80%) result from new mutations where neither parent has the condition. A parent with achondroplasia has a 50% chance of passing the gene to their child. How Many People Are Affected with Achondroplasia? Achondroplasia occurs in approximately 1 in every 15,000 to 40,000 live births worldwide. It affects males and females equally and is found in all ethnic groups. How Does Achondroplasia Affect My Child’s Body? Achondroplasia primarily affects the growth of long bones, resulting in shorter arms and legs. Other physical characteristics include a giant head with a prominent forehead, mid-face hypoplasia (underdeveloped mid-face), and a curved spine. These features can lead to various medical complications, such as breathing difficulties, obesity, and spinal stenosis. Symptoms and Causes Symptoms of achondroplasia include: The primary cause of achondroplasia is a mutation in the FGFR3 gene, which affects bone growth and development. Diagnosis and Tests Diagnosis of achondroplasia can be made through: Management and Treatment While there is no cure for achondroplasia, management focuses on addressing complications and improving quality of life. Treatment options include: Prevention Since most cases of achondroplasia result from new mutations, no known prevention exists. Genetic counselling can help prospective parents understand the risks and implications if there is a family history of the condition. Outlook / Prognosis With appropriate medical care and support, individuals with achondroplasia can lead fulfilling lives. Lifespan is typically average, although regular monitoring and treatment of complications are essential. Living With Living with achondroplasia involves ongoing medical care, physical adaptations, and social support. It’s important to foster an inclusive environment encouraging participation in various activities and providing emotional and psychological support. Engaging with support groups and organizations can also benefit individuals and their families. Achondroplasia presents unique challenges and requires a comprehensive approach to care. Understanding the condition and accessing the right medical and social support can significantly enhance the quality of life for affected individuals.

